Overview
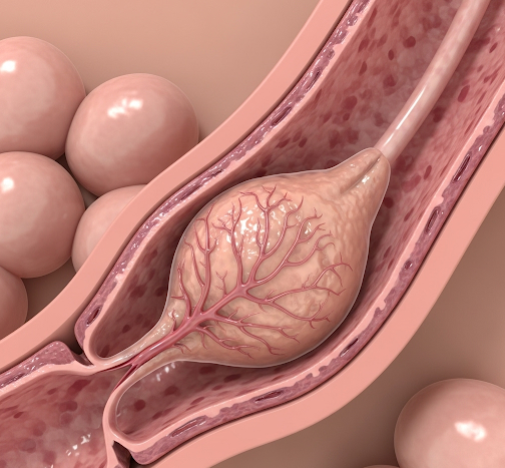
Intraductal papilloma is a benign tumor that develops within the milk ducts of the breast. It consists of papillary epithelial proliferations—finger-like projections lined by both epithelial and myoepithelial cells—that grow inside the lactiferous ducts. Although these growths are non-cancerous, they can cause symptoms such as nipple discharge or palpable lumps and occasionally harbor atypical or precancerous cells, making accurate diagnosis and management essential. In Korea, where breast cancer screening and care are highly advanced, intraductal papillomas are diagnosed early using sophisticated imaging and biopsy techniques, with minimally invasive surgical options available to effectively treat the condition while preserving breast aesthetics.
What is Intraductal Papilloma?
An intraductal papilloma originates from the epithelial cells lining the mammary ducts. These tumors create papillary fronds that protrude into the ductal lumen and secrete mucous or serous fluid. Papillomas can occur in two primary forms:
- Central (solitary) papillomas: Typically single lesions located in the larger, central ducts near the nipple. They are most often responsible for nipple discharge.
- Peripheral (multiple) papillomas: Occur in the smaller branch ducts further from the nipple and are more likely to be multiple. These are less often associated with discharge but may be more likely to contain atypical cells.
Intraductal papillomas are mostly benign but require evaluation because some may be associated with atypia or carcinoma in situ, especially when multiple or peripheral.
Symptoms
Many intraductal papillomas are asymptomatic and detected incidentally during imaging or investigations for nipple discharge. When symptoms are present, they include:
- Nipple discharge: This is the most common symptom. The discharge may be clear, serous, or bloody, often coming from a single duct. Blood-tinged discharge raises clinical suspicion and warrants further evaluation.
- Breast lump: Some patients notice a small, firm, well-circumscribed mass close to the nipple or deeper within the breast.
- Nipple pain or sensitivity: Mild discomfort or irritation around the nipple.
- Changes in nipple appearance: Retraction or inversion may rarely be observed.
- Occasionally, no symptoms: Detected on screening mammography or ultrasound.
Causes
The exact pathogenesis of intraductal papillomas is not fully understood, but several factors contribute:
- Hormonal influences: Estrogen and progesterone are believed to promote epithelial proliferation within the ducts.
- Ductal epithelial hyperplasia: Abnormal growth of ductal lining cells leads to papillary formation.
- Genetic mutations: While no specific mutations have been definitively linked, changes in cell-cycle regulation pathways may play a role.
- Age-related changes: These tumors most commonly develop in middle-aged women, possibly related to cumulative hormonal exposure.
Risk Factors
Risk factors for developing intraductal papilloma or associated atypia include:
- Age: Most frequently occurs in women aged 35 to 55 years.
- Hormonal therapy: Use of hormone replacement therapy (HRT) or oral contraceptives may increase risk.
- History of benign breast disease: Women with prior fibrocystic changes or other proliferative lesions may have higher susceptibility.
- Family history: A family history of breast cancer or papillomas may contribute.
- Multiple papillomas: These have a higher likelihood of harboring atypical cells or progressing to malignancy.
Complications
Although intraductal papillomas are benign, potential complications include:
- Atypical ductal hyperplasia or papillomatosis: Areas within the papilloma may show abnormal cellular proliferation that can be a precursor to cancer.
- Ductal carcinoma in situ (DCIS): Rarely, carcinoma cells may arise within the papilloma.
- Persistent or recurrent nipple discharge: Discomfort and social distress may result from ongoing symptoms.
- Papilloma recurrence: Though surgical excision is generally curative, recurrence is possible, especially if removal is incomplete.
- Infection or inflammation: Rare secondary infections may occur if ducts become obstructed.
Prevention
There is no specific way to prevent intraductal papillomas, but the following steps support early detection and reduce complications:
- Regular breast screening: Mammography and ultrasound examinations as recommended, especially in women over 40 or those with risk factors.
- Prompt evaluation of nipple discharge: Any persistent or bloody discharge should be assessed by a breast specialist.
- Healthy lifestyle: Maintaining hormonal balance through diet and exercise may have a protective effect.
- Avoidance of unnecessary hormone therapy: Minimizing exposure to exogenous hormones when possible.
Treatment Options in Korea
Korea is renowned for its excellence in breast healthcare, offering advanced diagnostic and therapeutic options for intraductal papillomas:
- Imaging Techniques:
- Mammography: To detect calcifications or masses, especially in women over 40.
- Breast Ultrasound: Highly effective for identifying intraductal masses and ductal dilatation.
- Ductography (Galactography): A specialized imaging test injecting contrast into the milk ducts to precisely locate papillomas causing nipple discharge.
- Magnetic Resonance Imaging (MRI): Used in complex or unclear cases to evaluate lesion extent.
- Biopsy and Histopathology:
- Core needle biopsy: Under ultrasound or ductoscopic guidance to obtain tissue for diagnosis.
- Excisional biopsy: Surgical removal of the papilloma and surrounding ductal tissue, often performed to rule out atypia or malignancy.
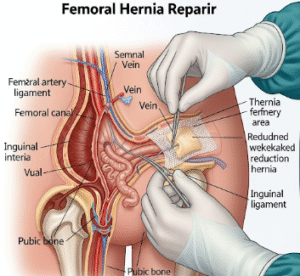
- Surgical Treatment:
- Microdochectomy: Removal of the involved duct and papilloma, often via a small incision under local or general anesthesia.
- Duct excision or segmental mastectomy: For multiple or complex lesions.
- Korean surgeons emphasize minimally invasive approaches to minimize scarring and preserve cosmetic appearance.
- Postoperative Care and Surveillance:
- Regular follow-up with breast imaging to monitor for recurrence or new lesions.
- Patient education on breast self-examination and awareness of symptoms.
- Multidisciplinary Approach:
Breast surgeons, radiologists, pathologists, and oncologists collaborate closely to ensure accurate diagnosis, effective treatment, and long-term monitoring. - Patient Support:
Korean medical centers provide counseling and support services to address the psychological impact of diagnosis and treatment.