Overview
Intraductal Papillary Mucinous Neoplasm (IPMN) is a type of cystic tumor that arises from the pancreatic ducts. It is characterized by the production of thick mucin and has the potential to progress from benign cystic lesions to invasive pancreatic cancer. IPMN is increasingly detected due to advanced imaging techniques and is considered a precancerous condition requiring careful monitoring or surgical intervention. In Korea, with its high standards of pancreatic care and diagnostic technology, patients diagnosed with IPMN benefit from comprehensive evaluation and personalized treatment plans aimed at preventing cancer progression while preserving pancreatic function.
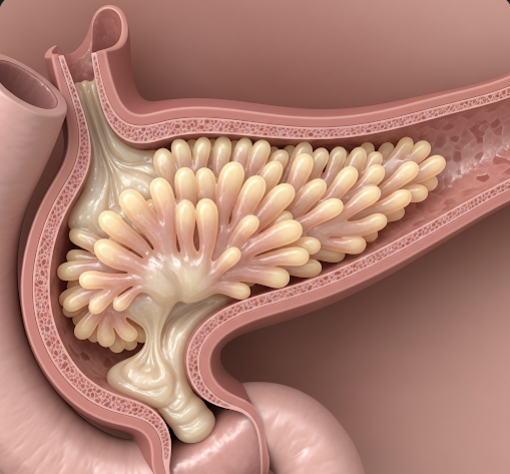
What is Intraductal Papillary Mucinous Neoplasm (IPMN)?
IPMN is a cystic lesion originating from the epithelial lining of the pancreatic ducts that produces mucin, a thick mucus-like substance. These tumors can involve the main pancreatic duct, its branch ducts, or both, and are classified accordingly into main-duct, branch-duct, or mixed types.
IPMNs cause dilation of the pancreatic ducts due to mucin accumulation and cellular proliferation. While some IPMNs remain benign, others have malignant potential and can transform into pancreatic adenocarcinoma if left untreated. This risk varies depending on the type and features of the lesion.
Symptoms
Many patients with IPMN are asymptomatic, and lesions are often discovered incidentally during imaging for other conditions. When symptoms occur, they may include:
- Abdominal discomfort or pain: Often vague or intermittent.
- Pancreatitis: Inflammation of the pancreas caused by duct obstruction due to mucin.
- Weight loss and loss of appetite: In advanced cases.
- Jaundice: If the bile duct is compressed.
- Nausea or vomiting: Occasionally reported.
- New-onset diabetes mellitus: Due to pancreatic dysfunction.
Causes
The exact cause of IPMN remains unclear, but several factors are implicated:
- Genetic mutations: Alterations in genes involved in cell growth and regulation.
- Chronic inflammation: Repeated pancreatic injury may predispose to IPMN development.
- Age: IPMN is more common in middle-aged and older adults.
- Environmental factors: Smoking and alcohol may contribute indirectly.
Risk Factors
Factors associated with higher risk or malignant transformation of IPMN include:
- Main-duct involvement: Main-duct IPMNs have a higher risk of malignancy compared to branch-duct types.
- Size of the cyst: Larger cysts (>3 cm) have increased cancer risk.
- Presence of mural nodules: Solid components inside cysts indicate possible malignancy.
- Symptoms: Symptomatic patients have a higher likelihood of malignant disease.
- Elevated tumor markers: Such as CA 19-9.
- Family history: Pancreatic cancer or hereditary syndromes.
Complications
If IPMN is left untreated or progresses, complications can include:
- Malignant transformation: Development of invasive pancreatic cancer, which has a poor prognosis.
- Pancreatitis: Due to duct obstruction.
- Obstruction of pancreatic or bile ducts: Leading to jaundice or digestive problems.
- Cyst rupture or infection: Rare but serious.
Prevention
There is no known way to prevent IPMN, but early detection and monitoring are key. Preventive strategies focus on:
- Regular health screenings: For at-risk individuals, including those with family history or symptoms.
- Lifestyle modifications: Avoiding smoking and excessive alcohol consumption.
- Management of pancreatic diseases: To reduce chronic inflammation.
Treatment Options in Korea
Korean medical centers specialize in the diagnosis and management of IPMN, providing state-of-the-art care:
- Accurate Diagnosis:
Advanced imaging techniques such as MRI with MRCP (magnetic resonance cholangiopancreatography), endoscopic ultrasound (EUS), and CT scans are routinely used. EUS allows fine-needle aspiration for cyst fluid analysis and cytology. - Risk Stratification:
Patients are evaluated based on cyst size, duct involvement, nodules, and symptoms to decide between surveillance and surgery. - Surveillance:
Low-risk, asymptomatic branch-duct IPMNs without worrisome features may be monitored with regular imaging and clinical follow-up. - Surgical Resection:
Indicated for high-risk lesions, main-duct IPMNs, or symptomatic cysts. Surgical options include pancreaticoduodenectomy, distal pancreatectomy, or total pancreatectomy, depending on lesion location. - Postoperative Care:
Korean hospitals provide multidisciplinary postoperative care to manage endocrine and exocrine pancreatic functions and prevent complications. - Research and Innovation:
Korea is involved in ongoing research on biomarkers and novel imaging techniques to improve early detection and treatment outcomes.