Overview
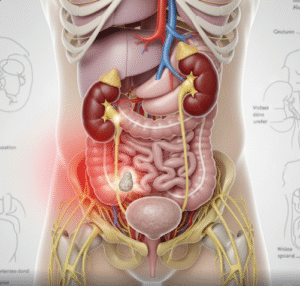
Inflammatory Bowel Disease (IBD) is a chronic and often debilitating group of disorders that cause inflammation of the gastrointestinal (GI) tract. The two primary types of IBD are Crohn’s disease and ulcerative colitis. Both conditions lead to persistent inflammation that damages the digestive tract lining, causing symptoms such as abdominal pain, diarrhea, and weight loss. IBD significantly affects the quality of life and may require lifelong management. In Korea, specialized gastroenterology centers offer comprehensive diagnostic and treatment services, combining the latest medical therapies and multidisciplinary care to improve patient outcomes.
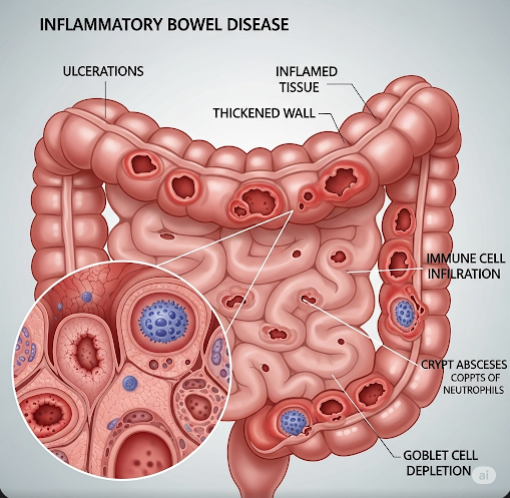
What is Inflammatory Bowel Disease (IBD)?
IBD is a term used to describe chronic inflammatory conditions of the GI tract with an autoimmune component. In Crohn’s disease, inflammation can affect any part of the GI tract from the mouth to the anus and typically involves all layers of the intestinal wall, often leading to patchy areas of damage with healthy tissue in between. Ulcerative colitis, on the other hand, primarily affects the colon and rectum, with inflammation limited to the innermost lining of the colon. Both diseases involve an abnormal immune response that mistakenly attacks the intestinal tissue.
Symptoms
The symptoms of IBD can vary depending on the disease type, location, and severity but commonly include:
- Chronic diarrhea: Often bloody, especially in ulcerative colitis.
- Abdominal pain and cramping: Usually in the lower abdomen but can occur anywhere along the digestive tract.
- Urgency and frequent bowel movements: Leading to discomfort and inconvenience.
- Weight loss and malnutrition: Due to poor nutrient absorption and loss of appetite.
- Fatigue: A common and debilitating symptom, often linked to anemia and chronic inflammation.
- Fever: Particularly during disease flares.
- Extraintestinal manifestations: Including joint pain, skin rashes, eye inflammation (uveitis), and liver disorders.
Causes
The exact cause of IBD remains unclear but is believed to result from a complex interaction of genetic, environmental, and immunological factors:
- Genetics: Multiple genes have been implicated in increasing susceptibility to IBD, with family history being a significant risk factor.
- Immune system dysfunction: The immune system mistakenly attacks the gut lining, causing chronic inflammation.
- Environmental triggers: These include diet, smoking (which worsens Crohn’s disease), infections, and use of certain medications such as NSAIDs.
- Gut microbiota imbalance: Alterations in the natural gut bacteria may contribute to disease onset and progression.
Risk Factors
- Having a first-degree relative with IBD increases risk.
- Age: IBD often begins in adolescence or early adulthood but can occur at any age.
- Smoking: Increases risk and severity in Crohn’s disease but may have a protective effect in ulcerative colitis.
- Living in urban or industrialized areas, possibly due to lifestyle or environmental exposures.
Complications
IBD can lead to numerous complications if not adequately managed:
- Intestinal strictures and obstruction: Resulting from chronic inflammation and scarring.
- Fistulas: Abnormal connections between the intestine and other organs or skin, common in Crohn’s disease.
- Colon cancer: Especially in patients with long-standing ulcerative colitis.
- Malnutrition and vitamin deficiencies: Due to impaired absorption.
- Severe bleeding and anemia.
- Extraintestinal complications: Such as arthritis, eye inflammation, and liver diseases like primary sclerosing cholangitis.
Prevention
While there is no sure way to prevent IBD, certain lifestyle choices may reduce risk or help manage symptoms:
- Smoking cessation.
- Healthy, balanced diet rich in fiber and low in processed foods.
- Stress management techniques.
- Avoiding unnecessary use of NSAIDs.
Treatment Options in Korea
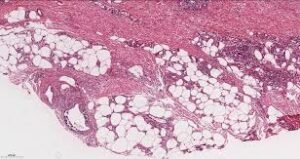
Diagnosis
Diagnosis typically involves a combination of:
- Colonoscopy and biopsy: To visualize inflammation and obtain tissue samples.
- Imaging studies: MRI, CT scans, and ultrasound to assess the extent and complications.
- Blood tests: To detect inflammation markers, anemia, and infection.
- Stool tests: To rule out infections and assess inflammation.
Medical Treatments
- Aminosalicylates (5-ASA): For mild to moderate ulcerative colitis.
- Corticosteroids: Used for short-term control during flares but not suitable for long-term use.
- Immunomodulators: Such as azathioprine and methotrexate, which suppress the immune response.
- Biologic agents: Including anti-TNF drugs (infliximab, adalimumab), integrin receptor antagonists, and newer small molecules like JAK inhibitors, which target specific inflammatory pathways.
- Antibiotics: Used in some cases, especially with abscesses or fistulas.
Surgical or Advanced Therapies
- Surgery may be required for complications such as strictures, fistulas, or uncontrolled disease.
- In ulcerative colitis, colectomy (removal of the colon) can be curative.
- Nutritional support, including enteral or parenteral nutrition, may be necessary during severe flares or malnutrition.
Rehabilitation and Support
- Korean IBD centers emphasize multidisciplinary care involving gastroenterologists, nutritionists, surgeons, and mental health professionals.
- Patient education focuses on medication adherence, dietary management, and monitoring symptoms.
- Support groups and counseling help patients cope with chronic disease stress.
Top Hospitals or Clinics in Korea
- Seoul National University Hospital – Gastroenterology Department
- Samsung Medical Center – Inflammatory Bowel Disease Clinic
- Asan Medical Center – Digestive Disease Center
- Yonsei Severance Hospital – Gastroenterology and Hepatology Division