Overview
Increased Intracranial Pressure (ICP) refers to the elevation of pressure inside the skull, which can result from various medical conditions affecting the brain. Elevated ICP is a critical and potentially life-threatening condition because the skull is a rigid structure that cannot expand, so increased pressure can compress brain tissue, reduce blood flow, and cause brain damage. In Korea, advanced neurology and neurosurgery centers employ state-of-the-art monitoring and treatment methods to manage ICP and improve patient outcomes.
What is Increased Intracranial Pressure (ICP)?
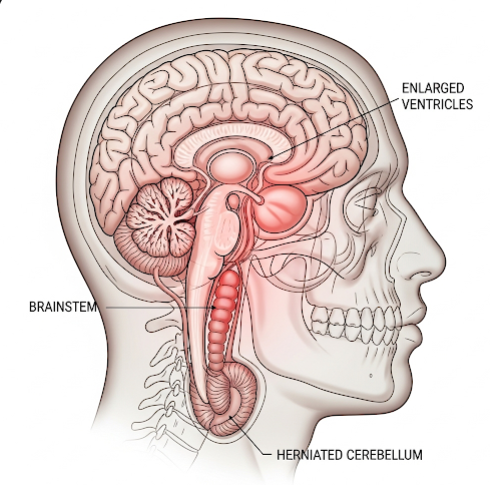
ICP is the pressure exerted by fluids such as cerebrospinal fluid (CSF) and blood within the cranial cavity. Normal ICP ranges between 7-15 mmHg in adults. When ICP rises above normal levels, it can compromise cerebral perfusion and cause brain herniation if untreated. Causes vary widely and include trauma, tumors, infections, and stroke.
Symptoms
- Headache, often worsening in the morning or with position changes
- Nausea and vomiting
- Visual disturbances such as blurred vision or double vision
- Papilledema (swelling of the optic disc) observed on eye exam
- Altered consciousness ranging from confusion to coma
- Seizures in some cases
- Changes in breathing pattern or heart rate in severe cases
Causes
- Traumatic brain injury (TBI)
- Brain tumors or abscesses
- Hydrocephalus (excess CSF accumulation)
- Cerebral hemorrhage or stroke
- Infections such as meningitis or encephalitis
- Idiopathic intracranial hypertension (increased pressure without clear cause)
Risk Factors
- Head trauma or recent neurosurgery
- Brain tumors or cysts
- Central nervous system infections
- Blood clotting disorders
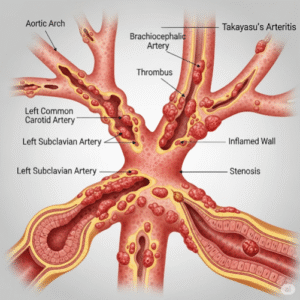
- High blood pressure or vascular abnormalities
Complications
- Brain herniation causing irreversible brain damage
- Permanent neurological deficits such as vision loss or paralysis
- Coma or death if untreated
- Secondary brain injury due to reduced blood flow
Prevention
- Prompt treatment of head injuries and infections
- Regular monitoring in patients with brain tumors or hydrocephalus
- Avoidance of activities that significantly increase ICP in vulnerable individuals
Treatment Options in Korea
Diagnosis
- Clinical neurological examination assessing consciousness and neurological signs
- Neuroimaging with CT or MRI to identify causes and brain swelling
- Direct ICP monitoring using intracranial pressure sensors in critical cases
- Ophthalmologic examination for papilledema
Medical Treatments
- Elevation of head to 30 degrees to improve venous drainage
- Osmotic diuretics such as mannitol or hypertonic saline to reduce brain swelling
- Controlled hyperventilation to lower carbon dioxide levels and reduce cerebral blood flow
- Sedation and pain control to prevent pressure spikes
- Treatment of underlying causes like infections or tumors
Surgical or Advanced Therapies
- Ventriculostomy or external ventricular drain to remove excess CSF
- Decompressive craniectomy to relieve pressure by removing part of the skull
- Removal of mass lesions such as tumors or hematomas
Rehabilitation and Support
- Intensive care monitoring in neurocritical units
- Physical and occupational therapy for neurological recovery
- Psychological support for patients and families
Top Hospitals or Clinics in Korea
- Seoul National University Hospital – Neurosurgery and Neurology Departments
- Samsung Medical Center – Neurocritical Care Unit
- Asan Medical Center – Brain Center
- Yonsei Severance Hospital – Neuroscience Institute