Overview
Inclusion Body Myositis (IBM) is a rare, progressive inflammatory muscle disease characterized by muscle weakness and wasting, primarily affecting adults over the age of 50. It is classified as an inflammatory myopathy with both autoimmune and degenerative features. IBM leads to difficulty in performing everyday activities like climbing stairs, gripping objects, and swallowing. In Korea, neuromuscular and rheumatology specialists provide advanced diagnostic techniques and multidisciplinary care to manage symptoms and improve quality of life for patients with IBM.
What is Inclusion Body Myositis?
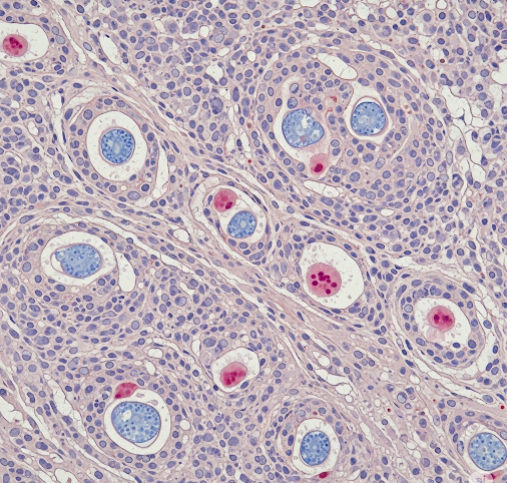
IBM is a chronic muscle disorder marked by inflammation, muscle fiber degeneration, and the presence of abnormal protein aggregates called inclusion bodies within muscle cells. The disease primarily affects the muscles of the thighs, wrists, and fingers, causing progressive weakness. Unlike other inflammatory myopathies, IBM tends to respond poorly to immunosuppressive treatments.
Symptoms
- Gradual onset of muscle weakness, especially in the quadriceps and forearm muscles
- Difficulty with tasks such as climbing stairs, rising from a chair, or gripping objects
- Frequent falls due to leg weakness
- Swallowing difficulties (dysphagia) in advanced stages
- Muscle wasting and atrophy visible over time
- Possible mild muscle pain or discomfort
Causes
- Exact cause is unknown but involves autoimmune inflammation and abnormal protein buildup in muscle cells
- Genetic susceptibility combined with environmental triggers may play a role
- Age-related degenerative changes also contribute to disease progression
Risk Factors
- Age over 50 years (most patients diagnosed after this age)
- Male gender is slightly more affected
- Family history is rare but possible in some cases
Complications
- Progressive disability due to muscle weakness
- Swallowing problems leading to malnutrition or aspiration pneumonia
- Reduced mobility increasing risk of falls and fractures
- Respiratory muscle involvement in advanced disease causing breathing difficulties
Prevention
- No known prevention due to unclear etiology
- Early diagnosis and supportive care can slow progression and improve quality of life
Treatment Options in Korea
Diagnosis
- Clinical examination noting characteristic pattern of muscle weakness
- Blood tests for muscle enzymes (elevated creatine kinase)
- Electromyography (EMG) to assess muscle electrical activity
- Muscle biopsy revealing inflammation, inclusion bodies, and protein aggregates
- MRI of muscles to detect inflammation and atrophy
Medical Treatments
- Immunosuppressive drugs generally show limited benefit but may be tried
- Physical therapy to maintain muscle strength and flexibility
- Occupational therapy to assist with daily activities
- Speech therapy for swallowing difficulties
- Nutritional support for patients with dysphagia
Surgical or Advanced Therapies
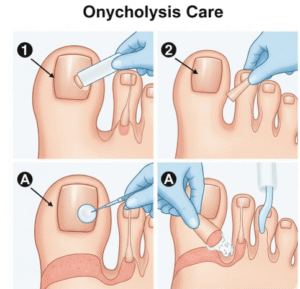
- Feeding tube placement (gastrostomy) in severe swallowing impairment
- Experimental therapies and clinical trials in specialized centers
Rehabilitation and Support
- Multidisciplinary approach including neurologists, physiotherapists, speech therapists, and dietitians
- Assistive devices like braces or walkers to aid mobility
- Psychological support for coping with chronic disease
Top Hospitals or Clinics in Korea
- Seoul National University Hospital – Neurology and Rheumatology Departments
- Samsung Medical Center – Neuromuscular Disease Clinic
- Asan Medical Center – Department of Neurology
- Yonsei Severance Hospital – Neurology and Rehabilitation Medicine