Overview
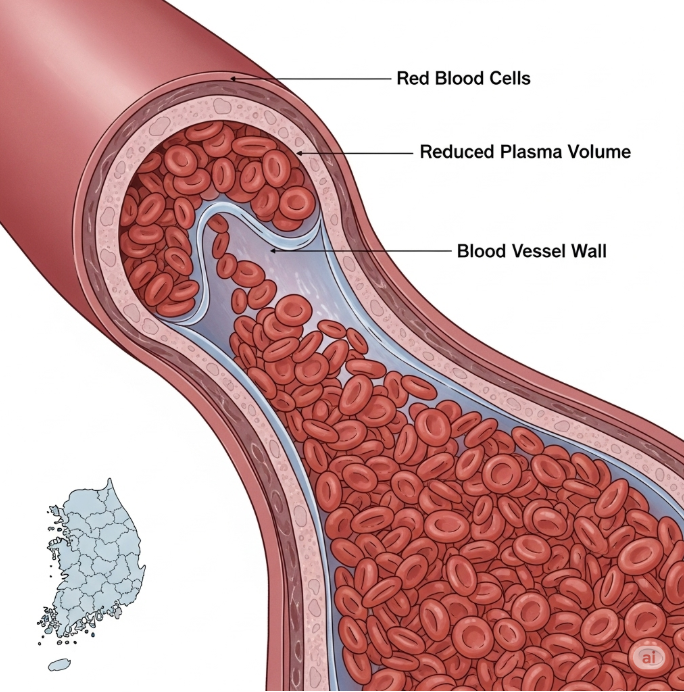
Hemoconcentration is a condition in which the proportion of red blood cells in the blood increases due to a reduction in plasma volume. It can result from dehydration, fluid loss, or other medical conditions affecting fluid balance. In Korea, hemoconcentration is commonly monitored in hospitals during emergency care, surgery, and treatment of illnesses like severe diarrhea or burns.
What is Hemoconcentration?
Hemoconcentration occurs when the blood becomes thicker due to reduced plasma, leading to higher hematocrit and hemoglobin levels. While often a temporary and reversible condition, hemoconcentration can increase the risk of blood clots and cardiovascular complications if left untreated.
Symptoms
- Dark-colored urine
- Dizziness or lightheadedness
- Fatigue or weakness
- Rapid heartbeat
- Headache
- Low blood pressure in severe cases
Causes
- Severe dehydration from vomiting, diarrhea, or excessive sweating
- Burns or extensive fluid loss
- Use of diuretics
- Shock or severe blood loss
- Underlying medical conditions affecting fluid balance (e.g., kidney or endocrine disorders)
Risk Factors
- Older adults (more prone to dehydration)
- Children (sensitive to fluid loss)
- Chronic kidney disease or diabetes
- Hot and humid environments (risk of heat-related dehydration)
- Patients on diuretics or medications affecting fluid balance
Complications
- Increased blood viscosity leading to thrombosis
- Stroke or heart attack due to reduced blood flow
- Organ damage from impaired perfusion
- Kidney injury due to reduced blood volume
- Dizziness, falls, and related injuries
Prevention
- Maintain proper hydration with water or electrolyte solutions
- Monitor fluid intake during illness or high temperatures
- Avoid excessive alcohol and caffeinated beverages
- Early medical evaluation for persistent vomiting or diarrhea
- Regular check-ups for individuals with chronic conditions
Treatment Options in Korea
Diagnosis
- Blood tests to check hematocrit, hemoglobin, and plasma volume
- Electrolyte panels to assess dehydration or fluid imbalance
- Urinalysis to evaluate kidney function
- Physical examination for signs of dehydration and fluid loss
Medical Treatments
- Intravenous (IV) fluids to restore plasma volume and correct electrolyte imbalance
- Oral rehydration solutions for mild cases
- Monitoring of vital signs and blood viscosity
- Treatment of underlying causes, such as kidney disease or endocrine disorders
Rehabilitation and Support
- Education on proper hydration
- Ongoing monitoring for patients with chronic illnesses
- Nutritional counseling to prevent recurrent fluid imbalances
- Follow-up testing to ensure normalization of hematocrit