Overview
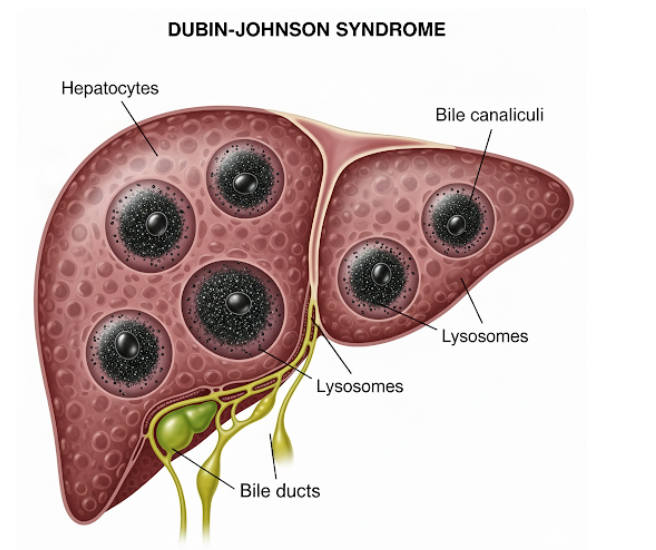
Dubin-Johnson Syndrome (DJS) is a rare genetic liver disorder characterized by chronic conjugated hyperbilirubinemia. In South Korea, although uncommon, awareness of DJS is important for differential diagnosis in patients presenting with jaundice. The condition is generally benign, but correct diagnosis prevents unnecessary treatment and anxiety.
What is Dubin-Johnson Syndrome?
Dubin-Johnson Syndrome is an inherited autosomal recessive disorder affecting the liver’s ability to excrete conjugated bilirubin into the bile. It usually presents in adolescence or early adulthood. Unlike other liver diseases, DJS typically does not cause liver damage, cirrhosis, or serious complications, but patients may experience intermittent jaundice.
Symptoms
The primary symptoms include:
- Mild to moderate jaundice (yellowing of skin and eyes)
- Dark urine due to increased bilirubin excretion
- Fatigue in some patients
- Occasionally abdominal discomfort
- Symptoms may worsen during illness, stress, or pregnancy
Causes
DJS is caused by mutations in the ABCC2 gene, which codes for a protein responsible for transporting conjugated bilirubin from liver cells into bile. This genetic defect leads to impaired bilirubin excretion and its accumulation in the bloodstream.
Risk Factors
Since DJS is genetic, risk factors include:
- Family history of Dubin-Johnson Syndrome
- Consanguineous marriages increasing autosomal recessive inheritance risk
Complications
DJS is generally benign, but potential issues include:
- Intermittent jaundice during stress or illness
- Rare association with gallstones due to chronic bilirubin increase
- Psychological impact of visible jaundice
Prevention
Being a genetic disorder, DJS cannot be prevented. However:
- Genetic counseling is advised for families with history of the syndrome
- Awareness helps avoid unnecessary liver biopsies or aggressive treatments
Treatment Options in Korea
There is no specific treatment for Dubin-Johnson Syndrome, as it is benign. Management in South Korea focuses on monitoring and supportive care:
Medical Management:
- Regular liver function tests to monitor bilirubin levels
- Avoidance of hepatotoxic drugs and alcohol
- Symptomatic care during episodes of jaundice
Supportive Measures:
- Patient education on the benign nature of the condition
- Guidance for lifestyle management to minimize stress-induced jaundice
Specialized Care:
- Hepatology departments in Korean hospitals provide diagnostic support, including liver function tests and genetic testing
- Genetic counseling is available for affected individuals and families
Early recognition in Korea ensures patients avoid unnecessary interventions and maintain a normal, healthy life despite intermittent jaundice.