Overview
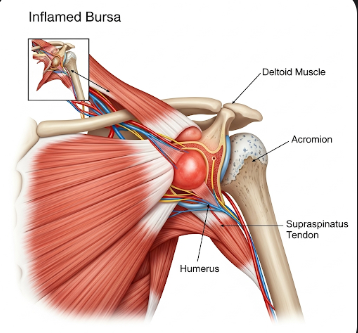
Bursitis is the inflammation of a bursa, a small fluid-filled sac that acts as a cushion between bones, tendons, and muscles. Bursae help reduce friction and facilitate smooth movement of joints. When inflamed, they can cause pain, swelling, and restricted mobility, often affecting the shoulder, elbow, hip, or knee.
In Korea, bursitis is treated in orthopedic and rehabilitation clinics using advanced imaging, physical therapy, medications, and minimally invasive procedures. Early intervention is emphasized to relieve pain, restore joint function, and prevent chronic inflammation.
What is Bursitis?
Bursitis occurs when a bursa becomes irritated or inflamed. The condition can be acute, developing suddenly after injury or overuse, or chronic, persisting over weeks to months.
Commonly affected bursae include:
- Subacromial bursa in the shoulder
- Olecranon bursa in the elbow
- Trochanteric bursa in the hip
- Prepatellar bursa in the knee
- Retrocalcaneal bursa in the heel
Bursitis can result in localized pain, swelling, redness, and difficulty moving the affected joint.
Symptoms
Symptoms of bursitis typically include:
- Localized joint pain that worsens with movement or pressure
- Swelling and tenderness over the affected bursa
- Warmth or redness in cases of infection
- Limited range of motion, making daily activities difficult
- Stiffness after periods of inactivity
- Gradual onset in chronic cases, or sudden pain after trauma or repetitive activity
In some cases, bursitis may mimic other joint conditions, requiring careful diagnosis.
Causes
Bursitis can be caused by mechanical, infectious, or systemic factors:
- Repetitive motion or overuse of joints, such as throwing, lifting, or kneeling
- Direct trauma or injury to a joint or surrounding tissue
- Infection, particularly in superficial bursae, leading to septic bursitis
- Underlying medical conditions, including rheumatoid arthritis, gout, or diabetes
- Age-related wear and tear, reducing bursa elasticity and resilience
- Postural or structural abnormalities, increasing pressure on specific joints
Risk Factors
- Occupation involving repetitive movements, such as carpentry, gardening, or sports
- Athletic activity, especially throwing, running, or cycling
- Age, as older adults are more prone to bursitis due to joint degeneration
- Medical conditions, such as arthritis, diabetes, or thyroid disorders
- Previous joint injuries, which may predispose bursae to inflammation
- Obesity, increasing mechanical stress on weight-bearing joints
Complications
If untreated, bursitis can lead to:
- Chronic pain and persistent inflammation
- Reduced joint mobility, affecting daily activities
- Calcification or thickening of the bursa
- Tendon damage or rupture due to ongoing irritation
- Septic bursitis, a serious infection requiring urgent medical care
- Secondary musculoskeletal problems, such as muscle imbalance or joint strain
Prevention
Bursitis prevention involves reducing stress on joints and maintaining joint health:
- Avoid repetitive movements or take frequent breaks during repetitive tasks
- Use proper techniques when lifting, bending, or exercising
- Wear protective gear or padding for joints during high-risk activities
- Maintain healthy body weight to reduce pressure on joints
- Strengthen muscles around joints through physical therapy or exercise
- Early treatment of minor injuries to prevent progression to bursitis
Treatment Options in Korea
Diagnosis
Diagnosis of bursitis in Korea involves clinical evaluation, imaging, and laboratory tests:
- Physical examination to assess swelling, tenderness, and joint range of motion
- Ultrasound or MRI to visualize inflamed bursae and rule out tendon involvement
- X-rays to exclude bone abnormalities
- Blood tests if infection or systemic inflammation is suspected
Medical Management
Initial management focuses on pain relief and inflammation reduction:
- Rest and activity modification to reduce stress on the affected joint
- Ice therapy to alleviate pain and swelling
- Non-steroidal anti-inflammatory drugs (NSAIDs) for pain control
- Oral antibiotics for septic bursitis
- Corticosteroid injections directly into the bursa to reduce inflammation
Interventional and Surgical Treatments
For persistent or severe bursitis:
- Aspiration of bursal fluid to reduce swelling and analyze for infection
- Arthroscopic bursectomy, a minimally invasive procedure to remove the inflamed bursa
- Open surgery in severe cases where conservative or minimally invasive measures fail
- Postoperative rehabilitation, including physical therapy to restore mobility
Supportive Care
- Physical therapy to strengthen surrounding muscles and prevent recurrence
- Stretching exercises to maintain joint flexibility
- Education on ergonomics and movement patterns to minimize stress on bursae
- Follow-up evaluations to monitor healing and prevent chronic inflammation
Prognosis
The prognosis of bursitis is generally favorable with early diagnosis and appropriate management:
- Acute bursitis often resolves within weeks with conservative treatment
- Chronic bursitis may require long-term management but can be controlled with therapy and lifestyle adjustments
- Surgical interventions in Korea have high success rates and minimize long-term complications
- With proper care, patients can regain full joint function, reduce pain, and prevent recurrence
Bursitis management in Korea combines advanced diagnostics, effective medical and surgical interventions, and rehabilitative support, ensuring optimal recovery and improved quality of life for patients suffering from this condition.