Overview
Body Dysmorphic Disorder (BDD) is a mental health condition characterized by obsessive preoccupation with perceived flaws in appearance, often minor or imagined. Individuals with BDD may spend hours each day examining, camouflaging, or trying to “fix” their perceived defects, significantly affecting daily life, social interactions, and emotional well-being.
In Korea, BDD is increasingly recognized within psychiatric and counseling services, particularly due to societal emphasis on appearance and beauty. Korean clinics offer psychotherapy, psychiatric evaluation, and support programs, while promoting early intervention to prevent severe complications like depression, social isolation, or self-harm.
What is Body Dysmorphic Disorder?
BDD is a psychological disorder where a person becomes excessively concerned about perceived physical imperfections. These concerns are often disproportionate to reality, and the individual may:
- Obsessively check mirrors or avoid mirrors entirely
- Compare their appearance with others frequently
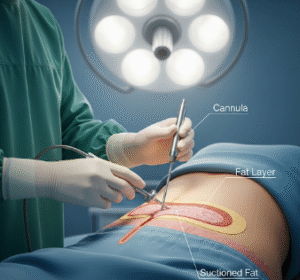
- Seek cosmetic procedures repeatedly
- Experience significant anxiety, depression, or social withdrawal
The disorder may focus on any body part, commonly the skin, hair, nose, or weight. BDD differs from normal self-consciousness due to its intensity, chronicity, and impact on daily functioning.
Symptoms
Symptoms of BDD may include:
- Preoccupation with perceived flaws for at least one hour per day
- Repetitive behaviors: mirror checking, skin picking, excessive grooming, or seeking reassurance
- Avoidance of social situations due to embarrassment
- Frequent comparison with others’ appearance
- Distress or impairment in personal, academic, or occupational life
- Mood disturbances: anxiety, depression, or irritability
- Suicidal thoughts or behaviors in severe cases
- Excessive use of cosmetics or cosmetic procedures
BDD often begins in adolescence or early adulthood and can persist for years without treatment.
Causes
The exact cause of BDD is multifactorial, including genetic, neurological, psychological, and environmental factors:
Genetic factors:
- Family history of BDD, obsessive-compulsive disorder (OCD), or depression increases risk
Neurological factors:
- Differences in brain areas responsible for perception, attention, and emotional regulation
Psychological factors:
- Low self-esteem or perfectionistic tendencies
- High sensitivity to criticism
- Cognitive distortions leading to exaggerated perception of flaws
Environmental factors:
- Childhood abuse, bullying, or teasing related to appearance
- Cultural and societal pressures emphasizing beauty or body image
- Media exposure and social comparison, particularly in appearance-focused environments
Risk Factors
- Adolescence or young adulthood: Typical onset period
- Family history: BDD, OCD, or mood disorders
- History of bullying or criticism about appearance
- Perfectionism or obsessive personality traits
- High exposure to appearance-focused media
- Psychosocial stressors: Peer pressure, academic, or occupational stress
Complications
Without treatment, BDD can result in severe complications:
- Depression and anxiety disorders
- Social isolation and withdrawal
- Impaired occupational or academic performance
- Repeated cosmetic procedures with little satisfaction
- Substance abuse to cope with emotional distress
- Self-harm or suicidal behavior
- Chronic stress and diminished quality of life
Prevention
While complete prevention may not be possible due to genetic and psychological factors, certain measures reduce severity or delay onset:
- Early education on healthy body image for children and adolescents
- Promoting resilience and self-esteem in school and family environments
- Awareness of media influence and unrealistic beauty standards
- Early psychological support for teens experiencing body dissatisfaction
- Screening for BDD in high-risk populations
- Family involvement in recognizing early signs of distress or obsessive behaviors
Treatment Options in Korea
Diagnosis
In Korea, BDD is diagnosed by psychiatrists or clinical psychologists through:
- Clinical interviews: Assessing preoccupation with appearance, distress, and functional impairment
- Psychometric scales: BDD-YBOCS (Yale-Brown Obsessive Compulsive Scale modified for BDD)
- Evaluation for coexisting disorders: Depression, anxiety, OCD, or eating disorders
- History and observation: Assessing behaviors such as mirror checking, skin picking, or avoidance
Psychotherapy
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and challenging distorted thoughts about appearance, reducing compulsive behaviors, and improving coping strategies
- Exposure and Response Prevention (ERP): Gradual exposure to feared social situations without performing appearance rituals
- Family therapy: Supports family members in understanding and managing BDD behaviors
- Mindfulness-based therapy: Reduces obsessive focus and anxiety related to appearance
Medical Management
- Selective Serotonin Reuptake Inhibitors (SSRIs): Commonly prescribed to reduce obsessive thoughts, anxiety, and depression
- Other antidepressants or medications: Considered in treatment-resistant cases
- Regular follow-up: Monitors effectiveness and side effects
Supportive Care
- Peer support groups: Provide encouragement and reduce feelings of isolation
- Lifestyle counseling: Emphasis on balanced routines, exercise, and stress management
- Education: Teaching patients to differentiate between realistic and distorted perceptions
- Monitoring for suicidal ideation: Crisis interventions when necessary
Prognosis
With early intervention and proper treatment, the prognosis for BDD in Korea is favorable:
- Psychotherapy and medication can significantly reduce symptoms and improve functioning
- Long-term management may be required due to the chronic nature of BDD
- Early recognition improves outcomes, reduces risk of self-harm, and enhances quality of life
- Patients who adhere to treatment plans often experience improved social relationships, occupational success, and emotional well-being