Overview
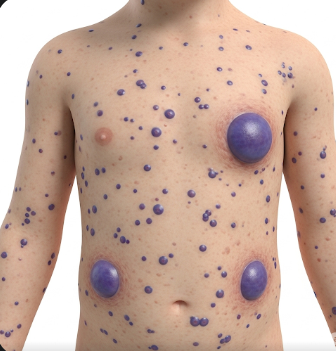
Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare vascular disorder characterized by multiple venous malformations (VMs) affecting the skin, gastrointestinal tract, and occasionally other organs. The lesions, often bluish and rubbery, can cause pain, bleeding, anemia, and functional impairments depending on their size and location.
In Korea, BRBNS is managed through specialized multidisciplinary care involving vascular surgeons, gastroenterologists, dermatologists, and interventional radiologists. Early detection, symptom management, and minimally invasive treatments are emphasized to improve quality of life and prevent complications.
What is Blue Rubber Bleb Nevus Syndrome?
BRBNS is a congenital vascular disorder characterized by multiple venous malformations:
- Skin lesions: Soft, compressible, blue-colored nodules, often visible at birth or in early childhood
- Gastrointestinal lesions: Can cause chronic bleeding and iron-deficiency anemia
- Other organ involvement: Rarely affects lungs, liver, spleen, or central nervous system
The syndrome is sporadic in most cases, although autosomal dominant inheritance has been reported in rare families. BRBNS differs from other vascular malformation syndromes because of its combination of cutaneous and visceral venous lesions, often leading to recurrent complications.
Symptoms
Symptoms vary depending on the location, number, and size of venous malformations:
Skin lesions:
- Blue or purple rubbery nodules
- Soft, compressible, and sometimes tender
- Often scattered over the trunk, limbs, and occasionally the face
- May increase in number or size over time
Gastrointestinal involvement:
- Chronic gastrointestinal bleeding
- Iron-deficiency anemia leading to fatigue and pallor
- Occult bleeding detected via stool tests
- Abdominal pain or discomfort in some cases
Other symptoms:
- Rarely, lesions in the lungs may cause shortness of breath or hemoptysis
- CNS involvement may lead to neurological deficits or seizures
- Recurrent pain at lesion sites
Causes
The exact cause of BRBNS is not fully understood, but it involves abnormal venous development during embryogenesis.
Genetic factors:
- Most cases are sporadic, but rare familial cases suggest autosomal dominant inheritance
- Mutations affecting vascular development pathways may play a role
Developmental factors:
- Abnormal formation of venous channels in the skin and internal organs
- Aberrant angiogenesis leads to multiple malformations that persist throughout life
Environmental or lifestyle factors do not appear to directly cause BRBNS, but trauma or irritation may exacerbate bleeding from lesions.
Risk Factors
- Family history: Rare autosomal dominant cases
- Congenital origin: Most patients present with lesions at birth or in early childhood
- Multiple vascular lesions: Individuals with more lesions have higher risk of anemia and complications
- Age: Gastrointestinal bleeding often presents later in childhood or adolescence
Complications
BRBNS can lead to various complications depending on the number and location of venous malformations:
- Chronic anemia: Due to recurrent gastrointestinal bleeding
- Pain and discomfort: Lesions may be tender or painful, especially in weight-bearing areas
- Functional impairment: Lesions on extremities can limit mobility or dexterity
- Internal organ bleeding: Rare but potentially life-threatening
- Infections: Secondary infections may occur if skin lesions ulcerate
- Psychosocial impact: Visible skin lesions may affect self-esteem and social interactions
Prevention
Since BRBNS is primarily congenital, prevention is limited. However, strategies focus on reducing complications and improving quality of life:
- Early detection and monitoring: Regular skin and gastrointestinal assessments
- Iron supplementation: Prevents or corrects iron-deficiency anemia
- Avoid trauma: Protect skin lesions from injury to reduce bleeding risk
- Routine follow-ups: Monitor growth and size of venous malformations
- Patient education: Recognizing signs of anemia, bleeding, or lesion complications
Treatment Options in Korea
Diagnosis
Korean medical centers utilize advanced diagnostic tools for BRBNS:
- Physical examination: Identifying cutaneous venous malformations
- Endoscopy: Detect gastrointestinal lesions and bleeding sources
- Imaging: MRI, CT scan, or ultrasound to assess deep tissue or organ involvement
- Laboratory tests: Hemoglobin, hematocrit, and iron studies to detect anemia
- Genetic counseling: In rare familial cases
Medical Management
- Iron supplementation: Corrects chronic anemia from gastrointestinal bleeding
- Pain management: Analgesics for painful or tender lesions
- Monitoring: Regular follow-up to detect new or enlarging lesions
Interventional and Surgical Management
- Laser therapy: Treats superficial skin lesions for cosmetic or symptomatic reasons
- Sclerotherapy: Injection of sclerosant into venous malformations to reduce size and bleeding
- Endoscopic intervention: Removal or ablation of gastrointestinal lesions to control bleeding
- Surgical excision: For large, symptomatic, or functionally impairing lesions
- Minimally invasive approaches: Preferred in Korea to reduce recovery time and complications
Supportive Care
- Multidisciplinary care involving dermatology, gastroenterology, and surgery
- Nutritional support to manage anemia and overall health
- Psychological counseling for self-esteem and coping with visible lesions
- Education on early signs of bleeding or complications for patients and caregivers
Prognosis
The prognosis for BRBNS in Korea depends on severity, lesion location, and access to specialized care:
- Skin lesions generally do not cause serious complications and can be managed with minor interventions
- Gastrointestinal lesions require monitoring and intervention to prevent chronic anemia and complications
- With modern diagnostic tools, interventional therapies, and multidisciplinary care available in Korea, patients can achieve improved quality of life, effective symptom management, and minimized risk of serious complications
- Long-term outcomes are favorable with ongoing surveillance and timely intervention, although complete cure is rare