Overview
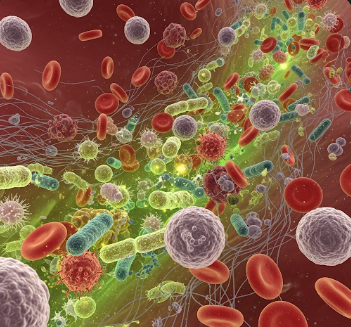
Blood poisoning, medically known as sepsis, is a life-threatening condition caused by the body’s extreme response to infection. When an infection spreads into the bloodstream, it can trigger widespread inflammation, organ dysfunction, and potentially septic shock. Sepsis is a medical emergency that requires immediate recognition and treatment to prevent multi-organ failure and death.
In Korea, hospitals offer state-of-the-art critical care units, rapid diagnostic testing, advanced antibiotic therapy, and supportive measures to manage sepsis. Public awareness and early medical intervention have significantly improved outcomes for patients with blood poisoning.
What is Blood Poisoning (Sepsis)?
Sepsis occurs when the body’s immune system overreacts to an infection, leading to systemic inflammation, tissue damage, and impaired blood flow. The condition can result from infections caused by bacteria, viruses, fungi, or parasites.
Sepsis is classified as:
- Sepsis: Presence of infection with systemic inflammatory response
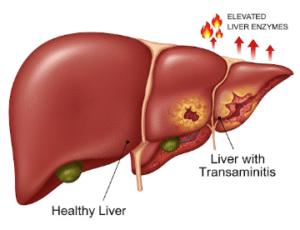
- Severe sepsis: Sepsis accompanied by organ dysfunction such as kidney failure, liver impairment, or low blood pressure
- Septic shock: Critically low blood pressure despite fluid resuscitation, leading to life-threatening complications
Early recognition and treatment are crucial because delays in intervention dramatically increase mortality risk.
Symptoms
Symptoms of sepsis may develop quickly or gradually, depending on the infection:
- High fever or low body temperature (hypothermia)
- Rapid heartbeat (tachycardia)
- Rapid breathing (tachypnea)
- Confusion, disorientation, or reduced alertness
- Extreme fatigue or weakness
- Low blood pressure, dizziness, or fainting
- Cold, clammy, or mottled skin
- Decreased urine output
- Chills, sweating, or shivering
- Signs of localized infection, such as redness, swelling, or pus
Symptoms can progress rapidly to severe sepsis or septic shock, emphasizing the need for urgent medical attention.
Causes
Blood poisoning can result from any type of infection that enters the bloodstream:
Bacterial infections (most common):
- Pneumonia
- Urinary tract infections
- Skin or soft tissue infections
- Intra-abdominal infections
Viral infections:
- Influenza
- COVID-19
- Other viral illnesses leading to secondary bacterial infections
Fungal infections:
- Candida species, especially in immunocompromised individuals
Other risk factors:
- Surgical or invasive procedures
- Open wounds or burns
- Indwelling medical devices such as catheters or intravenous lines
Risk Factors
- Age extremes: Infants, young children, and adults over 65
- Chronic illnesses: Diabetes, kidney disease, liver disease, or cardiovascular conditions
- Immunosuppression: Cancer treatment, HIV/AIDS, or steroid use
- Recent surgery or trauma
- Hospitalization: Particularly in intensive care units
- Invasive medical devices: Catheters, IV lines, or mechanical ventilation
- Delayed or inadequate treatment of infections
Complications
Sepsis can lead to serious complications, including:
- Septic shock: Critically low blood pressure causing organ failure
- Multi-organ failure: Kidney, liver, heart, and lung dysfunction
- Acute respiratory distress syndrome (ARDS): Severe lung impairment
- Blood clotting abnormalities: Disseminated intravascular coagulation (DIC)
- Amputations: In severe cases of tissue necrosis
- Long-term cognitive or physical impairment following recovery
- Death: Rapid progression if untreated
Prevention
Preventive strategies focus on infection control, early detection, and vaccination:
- Vaccination: Influenza, pneumococcal, meningococcal, and COVID-19 vaccines
- Hygiene practices: Handwashing, wound care, and sanitation
- Prompt treatment of infections: Early antibiotics for bacterial infections
- Regular health check-ups: Monitoring chronic conditions
- Hospital protocols: Sterile techniques for catheters, IV lines, and surgical procedures
- Healthy lifestyle: Proper nutrition, exercise, and immune system support
Treatment Options in Korea
Diagnosis
Korean hospitals use advanced diagnostic tools to rapidly identify sepsis:
- Blood cultures: Identify bacteria, viruses, or fungi in the bloodstream
- Laboratory tests: Complete blood count, lactate levels, kidney and liver function tests
- Imaging studies: CT, MRI, or ultrasound to locate sources of infection
- Vital signs monitoring: Continuous assessment of heart rate, blood pressure, and oxygen saturation
- Sepsis scoring systems: SOFA (Sequential Organ Failure Assessment) or qSOFA for early detection
Medical Management
- Intravenous antibiotics: Broad-spectrum initially, then targeted based on culture results
- Fluid resuscitation: IV fluids to maintain blood pressure and organ perfusion
- Vasopressors: Medications to raise blood pressure if fluids are insufficient
- Oxygen therapy: To maintain adequate oxygenation
- Supportive care: Pain management, fever control, and electrolyte balance
Surgical and Procedural Management
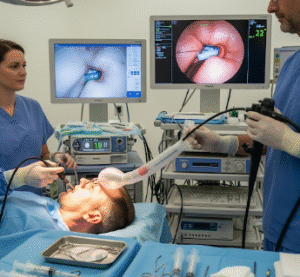
- Source control: Drainage of abscesses or removal of infected tissue
- Device removal: Catheters or prosthetic devices contributing to infection
- Advanced critical care interventions: Mechanical ventilation or dialysis in cases of organ failure
Supportive Care
- Continuous monitoring in intensive care units (ICUs)
- Nutritional support and hydration
- Rehabilitation and physical therapy for post-sepsis recovery
- Psychological counseling for post-traumatic stress or anxiety after critical illness
- Patient education on infection recognition and early hospital presentation
Prognosis
The prognosis for sepsis in Korea depends on early detection, underlying health, and the speed of intervention:
- Early recognition and treatment result in significantly higher survival rates
- Severe sepsis or septic shock carries higher mortality but is manageable with modern ICU care
- Long-term outcomes may include reduced physical strength or cognitive impairment, requiring rehabilitation
- Public awareness campaigns and advanced hospital protocols in Korea have improved survival and recovery rates for sepsis patients