Overview
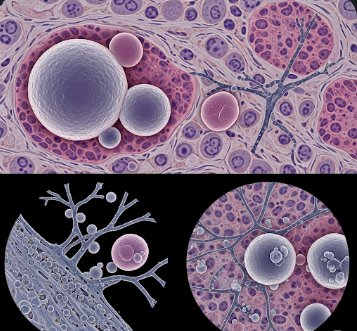
Blastomycosis is a rare fungal infection caused by the dimorphic fungus Blastomyces dermatitidis. This infection primarily affects the lungs but can also spread to the skin, bones, and other organs. Although blastomycosis is uncommon in Korea, international travel, immunocompromised individuals, and imported cases have led to occasional reports.
Korean medical centers with infectious disease specialists and advanced diagnostic tools provide early detection, antifungal therapy, and long-term follow-up. Awareness of this infection is crucial, especially for travelers returning from endemic regions such as North America, where the fungus is more prevalent.
What is Blastomycosis?
Blastomycosis is a systemic fungal infection acquired when fungal spores are inhaled into the lungs. In most cases, the infection begins as a pulmonary condition, ranging from mild respiratory symptoms to severe pneumonia. In some instances, the fungus can disseminate through the bloodstream, affecting the skin, bones, genitourinary system, or central nervous system.
Blastomycosis is classified into:
- Pulmonary blastomycosis: Primary lung infection
- Disseminated blastomycosis: Spread to skin, bones, and other organs
- Acute or chronic forms: Depending on disease progression and immune response
Symptoms
Symptoms of blastomycosis vary depending on infection severity and organ involvement:
Pulmonary symptoms:
- Persistent cough, sometimes with sputum
- Fever, chills, and fatigue
- Shortness of breath or chest discomfort
- Night sweats or weight loss
Disseminated symptoms:
- Skin lesions: Wart-like or ulcerative lesions, often on the face, hands, or limbs
- Bone pain or swelling due to skeletal involvement
- Urinary symptoms if the genitourinary system is affected
- Neurological symptoms in rare cases, such as headaches or confusion
Symptoms can be misdiagnosed as bacterial pneumonia, tuberculosis, or other fungal infections, making accurate diagnosis essential.
Causes
Blastomycosis is caused by inhaling spores of Blastomyces dermatitidis, which thrive in:
- Moist soil enriched with decaying organic matter
- Riverbanks and wooded areas in endemic regions
- Environmental exposure during outdoor activities such as camping, hiking, or construction
Once inhaled, the spores transform into yeast in the lungs, leading to infection. Individuals with weakened immune systems are at higher risk of severe or disseminated disease.
Risk Factors
- Travel or residence in endemic areas, particularly North America
- Immunocompromised conditions, such as HIV/AIDS, organ transplantation, or long-term steroid use
- Chronic lung diseases, including COPD or asthma
- Male gender, as some studies report higher incidence in men
- Outdoor exposure to soil or decaying vegetation, especially during activities that aerosolize spores
Complications
Blastomycosis can lead to several complications if untreated:
- Severe pneumonia leading to respiratory failure
- Disseminated infection affecting the skin, bones, or central nervous system
- Chronic lung disease due to persistent infection
- Septicemia or systemic spread in immunocompromised patients
- Death, although rare with timely treatment, particularly in severe or untreated cases
Prevention
Prevention strategies focus on reducing exposure to fungal spores:
- Avoid endemic areas when possible, especially moist soil-rich environments
- Protective clothing: Masks, gloves, and long sleeves when handling soil or decaying organic matter
- Avoid aerosolizing soil: Minimize activities that disturb contaminated soil
- Prompt medical attention: Seek early evaluation for persistent respiratory symptoms after travel to endemic regions
- Monitor immunocompromised individuals for early signs of infection
Treatment Options in Korea
Diagnosis
Accurate diagnosis in Korea involves several advanced techniques:
- Microscopic examination: Detecting yeast forms in tissue or sputum samples
- Culture: Fungal culture from respiratory secretions, tissue, or biopsy samples
- Histopathology: Skin or tissue biopsy for disseminated infection
- Imaging: Chest X-ray or CT scans to evaluate lung involvement
- Serological and molecular tests: Support diagnosis and differentiate from other fungal infections
Medical Management
Treatment primarily involves antifungal therapy:
- Mild to moderate pulmonary blastomycosis: Oral antifungals such as itraconazole for several months
- Severe or disseminated disease: Intravenous antifungals such as amphotericin B followed by oral itraconazole
- Treatment duration: Typically 6–12 months depending on severity, immune status, and organ involvement
- Supportive care: Oxygen therapy, hydration, and symptom management for severe pulmonary cases
Rehabilitation and Support
- Regular follow-up to monitor treatment response and detect recurrence
- Pulmonary rehabilitation for persistent respiratory symptoms
- Nutritional support and general health optimization during prolonged therapy
- Counseling and education for patients and families regarding infection control and prevention of reinfection
Prognosis
With timely diagnosis and appropriate antifungal therapy, blastomycosis has a favorable prognosis:
- Mild pulmonary infections often resolve completely with oral therapy
- Disseminated or severe infections require prolonged therapy but can still achieve complete remission
- Immunocompromised patients may experience higher risk of complications or prolonged recovery
- In Korea, advanced diagnostic facilities, access to effective antifungal medications, and specialized infectious disease care ensure optimal outcomes