Overview
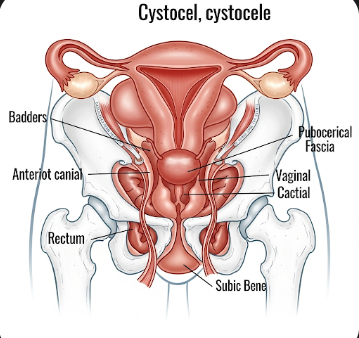
Bladder prolapse, medically known as cystocele, occurs when the bladder descends from its normal position into the vaginal wall due to weakening of the pelvic floor muscles and connective tissues. It is a common type of pelvic organ prolapse in women, particularly after childbirth, menopause, or chronic straining.
In Korea, awareness, early diagnosis, and access to pelvic floor specialists, urogynecologists, and advanced surgical options have improved outcomes for women with bladder prolapse. Treatment focuses on symptom relief, functional restoration, and prevention of recurrence.
What is Bladder Prolapse?
Bladder prolapse occurs when the supporting structures of the bladder weaken, causing it to bulge into the vaginal wall. It may be categorized into different grades based on severity:
- Mild: Minimal bulging with few or no symptoms
- Moderate: Noticeable bulge causing urinary discomfort or pelvic pressure
- Severe: Significant descent causing bladder dysfunction, urinary incontinence, or difficulty with urination
Bladder prolapse can affect urinary, sexual, and pelvic health, impacting daily life and quality of life.
Symptoms
Symptoms vary depending on the severity of prolapse:
- Vaginal bulge: Feeling of a lump or fullness in the vaginal area
- Pelvic pressure or heaviness
- Urinary problems: Difficulty starting urination, incomplete emptying, frequent urination, or urgency
- Urinary incontinence: Leakage of urine during activity, coughing, or sneezing
- Discomfort during sexual activity
- Lower back or pelvic pain
- Recurrent urinary tract infections due to incomplete bladder emptying
Early detection is essential for preventing worsening symptoms and associated complications.
Causes
Bladder prolapse develops due to weakening of pelvic floor support:
- Childbirth trauma: Vaginal delivery, especially multiple births or large babies
- Aging and menopause: Decreased estrogen weakens pelvic tissues
- Chronic straining: Constipation or heavy lifting increases intra-abdominal pressure
- Obesity: Extra weight strains pelvic muscles
- Previous pelvic surgery: Hysterectomy or other surgeries affecting pelvic support
- Genetic predisposition: Family history of weak connective tissue
Risk Factors
- Female gender, particularly postmenopausal women
- Multiple vaginal deliveries or complicated childbirth
- Chronic constipation or straining during bowel movements
- Obesity or high body mass index (BMI)
- Previous pelvic surgery, including hysterectomy
- Chronic coughing or respiratory conditions that increase abdominal pressure
- Connective tissue disorders, such as Ehlers-Danlos syndrome
Complications
Untreated bladder prolapse can lead to various complications:
- Urinary retention: Difficulty fully emptying the bladder, leading to infections or stones
- Recurrent urinary tract infections (UTIs)
- Urinary incontinence affecting daily activities
- Vaginal ulceration: Due to chronic pressure and friction of prolapsed tissue
- Sexual dysfunction: Pain or discomfort during intercourse
- Progressive prolapse: Worsening symptoms and increased risk of affecting other pelvic organs
Prevention
Preventive strategies focus on strengthening the pelvic floor and minimizing strain:
- Pelvic floor exercises (Kegels): Strengthen vaginal and bladder support muscles
- Healthy weight management: Reduce intra-abdominal pressure
- Avoid heavy lifting: Minimize repetitive strain on pelvic muscles
- Manage constipation: High-fiber diet and hydration to prevent straining
- Estrogen therapy: In postmenopausal women, topical estrogen may improve tissue strength
- Routine gynecological check-ups: Early detection and intervention
Treatment Options in Korea
Diagnosis
Korean healthcare providers use several methods to diagnose bladder prolapse accurately:
- Physical examination: Assessment of vaginal walls and bladder support
- Pelvic ultrasound: Visualizes the bladder and surrounding tissues
- Urodynamic studies: Evaluate bladder function, urine flow, and pressure
- Cystoscopy: Examines the bladder lining for complications
- MRI or advanced imaging: In severe or complex cases
Medical Management
- Lifestyle modifications: Weight management, avoiding straining, and proper bowel habits
- Pelvic floor physical therapy: Regular Kegel exercises and guided therapy
- Pessary devices: Removable vaginal devices to support the bladder and reduce prolapse
- Estrogen therapy: Topical estrogen creams may strengthen tissues in postmenopausal women
Surgical Management
Surgery is recommended for moderate to severe prolapse or persistent symptoms:
- Anterior colporrhaphy: Repair of vaginal wall and bladder support
- Mesh repair: Reinforces weakened tissues (used cautiously due to potential complications)
- Minimally invasive laparoscopic or robotic procedures: Reduced recovery time and improved precision
- Urinary diversion or concomitant anti-incontinence procedures: For women with severe urinary dysfunction
Rehabilitation and Support
- Post-surgical pelvic floor exercises to maintain bladder support
- Education on lifestyle changes to prevent recurrence
- Regular follow-up visits with urogynecologists
- Support groups for women with pelvic organ prolapse to improve quality of life
Prognosis
The prognosis for bladder prolapse in Korea is favorable with early detection and proper treatment:
- Mild cases managed with exercises or pessaries often experience symptom relief without surgery
- Surgical correction provides long-term improvement for moderate to severe prolapse
- Recurrence is possible, but ongoing pelvic floor care and lifestyle adjustments significantly reduce the risk
- Access to Korea’s advanced urogynecology services ensures comprehensive care, minimizing complications and improving quality of life