Overview
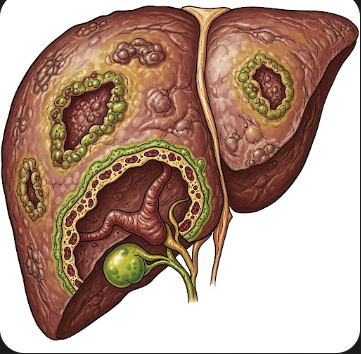
Biliary Cirrhosis is a chronic liver disease characterized by progressive destruction of the bile ducts, leading to bile accumulation, liver inflammation, and eventual fibrosis and cirrhosis. There are two primary forms: Primary Biliary Cirrhosis (PBC), an autoimmune condition, and Secondary Biliary Cirrhosis, which occurs due to prolonged bile duct obstruction from gallstones, tumors, or strictures.
In Korea, advanced hepatology clinics provide early detection, medical management, and liver transplantation for advanced cases. With timely diagnosis and treatment, patients can slow disease progression, manage symptoms, and maintain a higher quality of life.
What is Biliary Cirrhosis?
Biliary Cirrhosis involves damage and scarring of the bile ducts inside the liver. Bile, which aids digestion and removes toxins, builds up when the ducts are damaged. This accumulation leads to inflammation, liver cell injury, and eventually cirrhosis.
Primary Biliary Cirrhosis (PBC) is autoimmune in nature, predominantly affecting middle-aged women, whereas Secondary Biliary Cirrhosis results from identifiable causes of bile obstruction. Both types can lead to portal hypertension, liver failure, and the need for transplantation if untreated.
Symptoms
Symptoms of biliary cirrhosis may appear gradually and include:
- Fatigue and general weakness
- Itching (pruritus) due to bile salt accumulation
- Jaundice (yellowing of skin and eyes)
- Dark urine and pale stools
- Abdominal discomfort or right upper quadrant pain
- Swelling of the legs or abdomen due to fluid retention
- Bone pain and osteoporosis in chronic cases
- Easy bruising or bleeding due to impaired liver function
In advanced disease, complications such as ascites, hepatic encephalopathy, and variceal bleeding may occur.
Causes
The causes of biliary cirrhosis vary by type:
Primary Biliary Cirrhosis (PBC):
- Autoimmune attack on the small intrahepatic bile ducts
- Association with other autoimmune disorders, such as thyroid disease or Sjögren’s syndrome
Secondary Biliary Cirrhosis:
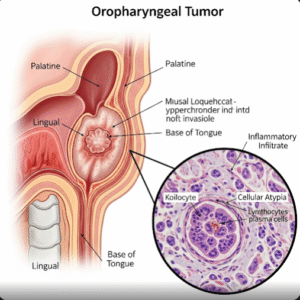
- Bile duct obstruction due to gallstones, strictures, or tumors
- Chronic pancreatitis affecting bile flow
- Post-surgical bile duct injury
Risk Factors
- Middle-aged women (for PBC)
- Family history of autoimmune liver disease
- History of gallstones or biliary obstruction (for secondary form)
- Coexisting autoimmune conditions
- Chronic liver disease or repeated bile duct infections
Complications
Without treatment, biliary cirrhosis can lead to severe complications:
- Liver cirrhosis and hepatic failure
- Portal hypertension, leading to varices and gastrointestinal bleeding
- Ascites and fluid accumulation in the abdomen
- Osteoporosis due to impaired vitamin D metabolism
- Fatigue and malnutrition from fat malabsorption
- Increased risk of hepatocellular carcinoma in long-term disease
Prevention
Prevention of biliary cirrhosis focuses on:
- Prompt treatment of gallstones, bile duct obstructions, or chronic infections
- Early screening for autoimmune liver disease in high-risk individuals
- Avoiding hepatotoxic medications and alcohol to reduce liver stress
- Maintaining healthy liver function through diet and regular medical check-ups
- Genetic counseling for families with a history of autoimmune liver disorders
Treatment Options in Korea
Diagnosis
Korean hepatology centers utilize advanced diagnostic methods:
- Blood tests including liver function tests and antimitochondrial antibodies (for PBC)
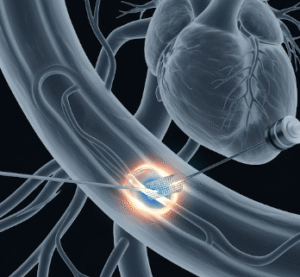
- Ultrasound and MRCP (Magnetic Resonance Cholangiopancreatography) to visualize bile ducts
- Liver biopsy to confirm fibrosis and cirrhosis stage
- Imaging studies to detect obstruction, stones, or tumors
- Bone density scans for assessing osteoporosis risk
Medical Management
- Ursodeoxycholic acid (UDCA): First-line therapy for PBC to improve bile flow and reduce liver damage
- Obeticholic acid: Used for patients not responding fully to UDCA
- Immunosuppressive medications in select autoimmune-related cases
- Symptom management: Antihistamines for itching, vitamin supplementation, and pain management
- Treatment of complications: Diuretics for ascites, beta-blockers for portal hypertension
Surgical and Interventional Procedures
- Endoscopic or surgical intervention to relieve bile duct obstruction in secondary biliary cirrhosis
- Liver transplantation for patients with end-stage liver disease or severe complications
- Korean transplant centers provide high survival rates and post-operative care tailored to pediatric and adult patients
Rehabilitation and Support
- Nutritional counseling to manage fat malabsorption and maintain bone health
- Regular monitoring of liver function, imaging, and bone density
- Patient education on disease progression, symptom monitoring, and adherence to medications
- Psychological support to manage chronic illness and lifestyle adjustments
Prognosis
With early diagnosis and appropriate medical management, patients with primary biliary cirrhosis in Korea can have a favorable prognosis, with slowed disease progression and improved quality of life. Secondary biliary cirrhosis outcomes depend on timely relief of obstruction and management of underlying causes. Liver transplantation remains a definitive option for advanced disease, with excellent outcomes in specialized Korean hepatology centers.