Overview
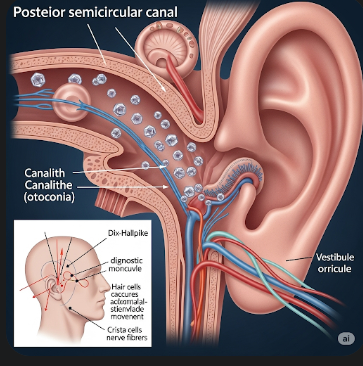
Benign Paroxysmal Positional Vertigo (BPPV) is a common inner ear disorder that causes brief episodes of spinning dizziness, often triggered by changes in head position. The term “benign” indicates that the condition is not life-threatening, and “paroxysmal” refers to the sudden onset of symptoms. BPPV occurs when tiny calcium crystals called otoconia become dislodged from the utricle within the inner ear and move into the semicircular canals, disrupting the normal flow of fluid and sending false signals about head movement to the brain.
In Korea, BPPV is widely diagnosed and treated in both outpatient and specialized vestibular clinics. Early recognition and intervention can provide rapid relief and prevent falls or injuries, which is particularly important for elderly patients.
What is Benign Paroxysmal Positional Vertigo?
BPPV is a disorder of the vestibular system, which controls balance and spatial orientation. The displaced otoconia within the semicircular canals interfere with the inner ear’s ability to accurately detect movement, leading to brief but intense vertigo episodes. These episodes typically last a few seconds to a minute and are triggered by specific head movements, such as looking up, rolling over in bed, or bending forward.
BPPV does not indicate a structural brain problem, and while it can recur, it is generally considered a self-limiting and treatable condition.
Symptoms
Common symptoms of BPPV include:
- Sudden episodes of spinning vertigo, often triggered by head movement
- Loss of balance or unsteadiness
- Nausea or vomiting during vertigo episodes
- Dizziness lasting seconds to minutes
- Lightheadedness between attacks in some cases
- Difficulty walking safely, especially in older adults
- Nystagmus (rapid involuntary eye movements) observed during diagnostic tests
Causes
BPPV occurs when otoconia crystals detach from the utricle and move into one of the semicircular canals. Causes and contributing factors include:
- Age-related degeneration of inner ear structures (most common in older adults)
- Head trauma or sudden impact
- Inner ear disorders such as labyrinthitis or vestibular neuritis
- Prolonged bed rest or limited movement
- Less commonly, BPPV can be idiopathic, with no identifiable cause
Risk Factors
Risk factors that increase the likelihood of BPPV include:
- Age over 50 years
- History of head injury or whiplash
- Previous episodes of inner ear infection or vestibular disorders
- Prolonged immobilization or surgery requiring extended bed rest
- Female gender (slightly higher prevalence reported)
Complications
While BPPV is benign, it can lead to:
- Falls and injuries, especially in elderly patients
- Fear of movement or anxiety about recurrence
- Disruption of daily activities due to unpredictable vertigo attacks
- Rarely, persistent vertigo if left untreated
Prevention
Though not all cases of BPPV can be prevented, the following strategies may reduce risk or recurrence:
- Avoiding sudden or extreme head movements, particularly in older adults
- Performing vestibular exercises or balance training
- Using caution when rising from bed or bending forward quickly
- Treating underlying inner ear infections promptly
- Maintaining good overall ear and balance health
Treatment Options in Korea
Diagnosis
Korean clinics follow a structured approach to confirm BPPV:
- Medical history focusing on vertigo triggers and duration
- Dix-Hallpike maneuver to detect positional vertigo and nystagmus
- Supine roll test for horizontal canal involvement
- Audiometric and vestibular tests to rule out other inner ear disorders
Canalith Repositioning Maneuvers
The mainstay of BPPV treatment involves repositioning maneuvers to guide displaced otoconia back to the utricle:
- Epley maneuver for posterior canal BPPV
- Semont maneuver for rapid canal repositioning
- Barbecue roll maneuver for horizontal canal BPPV
These procedures are highly effective, with symptom resolution in most patients after one or a few sessions.
Medications
Medications are rarely needed but may be used temporarily to manage:
- Nausea and vomiting (antiemetics)
- Severe vertigo during acute episodes
Medications do not treat the underlying cause but help reduce discomfort during attacks.
Vestibular Rehabilitation
- Balance and gaze stabilization exercises to strengthen the vestibular system
- Tai Chi or physiotherapy-based balance training in Korean rehabilitation centers
- Programs often include guided exercises and home routines to prevent recurrence
Surgical Options
Surgery is rarely required but may be considered in chronic, treatment-resistant BPPV:
- Posterior canal occlusion — a minimally invasive procedure to block the affected semicircular canal
Patient Education and Follow-Up
Korean specialists emphasize patient education:
- Understanding triggers and recognizing early symptoms
- Learning home repositioning exercises under professional guidance
- Scheduling periodic follow-ups to monitor balance and prevent falls
Prognosis
The prognosis for BPPV is excellent. Most patients experience full recovery within days to weeks after appropriate repositioning maneuvers. Recurrence is possible, but timely treatment ensures minimal impact on daily life. Elderly patients benefit from combined vestibular therapy and balance exercises to reduce the risk of falls.