Overview
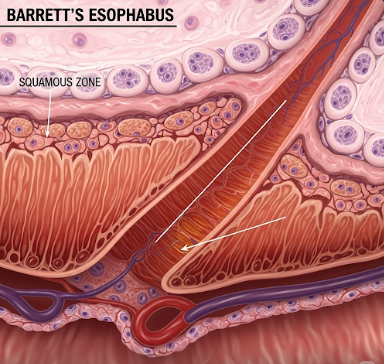
Barrett’s Esophagus (BE) is a medical condition in which the normal lining of the esophagus—the tube connecting the mouth to the stomach—is replaced by tissue similar to the lining of the intestine. This process, called intestinal metaplasia, usually develops as a response to chronic injury caused by acid reflux or gastroesophageal reflux disease (GERD). Although Barrett’s Esophagus itself does not always cause symptoms, it is considered a precancerous condition, as it increases the risk of developing esophageal adenocarcinoma, a type of esophageal cancer.
In Korea, advanced gastroenterology clinics and hospitals provide comprehensive care for Barrett’s Esophagus. Korean gastroenterologists are highly skilled in endoscopic diagnosis, surveillance, and minimally invasive treatment, allowing for early detection and intervention to prevent cancer progression. Patients benefit from personalized treatment plans, lifestyle counseling, and ongoing monitoring to manage both symptoms and risks.
What is Barrett’s Esophagus?
Barrett’s Esophagus occurs when the normal squamous epithelial lining of the lower esophagus is replaced with columnar epithelium, which is more resistant to acid but more prone to dysplasia and malignancy. The condition typically arises in individuals with long-standing GERD, as repeated exposure to stomach acid damages the esophageal lining and triggers cellular changes.
The severity of Barrett’s Esophagus can vary:
- Non-dysplastic Barrett’s Esophagus: No precancerous changes, but surveillance is necessary.
- Low-grade dysplasia: Early precancerous changes are present.
- High-grade dysplasia: Severe precancerous changes with a high risk of progression to esophageal adenocarcinoma.
Early detection and regular monitoring are crucial for preventing progression to cancer.
Symptoms
Barrett’s Esophagus itself often does not cause unique symptoms, but it is usually associated with GERD symptoms, such as:
- Frequent heartburn or acid reflux
- Regurgitation of sour or bitter-tasting stomach contents
- Difficulty or pain while swallowing (dysphagia)
- Chest discomfort or burning sensation
- Chronic cough, hoarseness, or sore throat in some patients
- Nausea or indigestion
Patients may not recognize Barrett’s Esophagus until an endoscopic examination is performed for persistent reflux symptoms.
Causes
The primary cause of Barrett’s Esophagus is chronic gastroesophageal reflux, which exposes the lower esophagus to stomach acid over long periods. Other contributing factors include:
- GERD: The strongest risk factor for developing BE.
- Obesity: Particularly abdominal obesity, which increases intra-abdominal pressure and reflux.
- Hiatal hernia: Displacement of the stomach into the chest can promote reflux.
- Smoking: Increases risk of Barrett’s Esophagus and esophageal cancer.
- Age and Gender: More common in adults over 50, particularly men.
- Genetic predisposition: Family history of BE or esophageal cancer may increase risk.
Risk Factors
Several factors heighten the likelihood of developing Barrett’s Esophagus:
- Long-standing GERD: Symptoms lasting more than 5–10 years
- Male gender: Men are more frequently affected than women
- Age over 50: Incidence rises with age
- Obesity and high-fat diet: Lifestyle factors that exacerbate reflux
- Smoking and alcohol use: Contributing to esophageal mucosal damage
- Ethnicity: More common among Caucasians compared to other ethnic groups
Complications
Barrett’s Esophagus increases the risk of serious complications if not managed properly:
- Esophageal adenocarcinoma: The most significant risk; risk is higher with dysplasia.
- Strictures: Narrowing of the esophagus due to chronic inflammation and scarring, leading to swallowing difficulties.
- Ulcers: Open sores in the esophagus caused by persistent acid exposure.
- Bleeding: In rare cases, erosions or ulcers may bleed, causing anemia or other complications.
- Progression of dysplasia: Low-grade dysplasia can advance to high-grade dysplasia, increasing cancer risk.
Early detection, surveillance, and intervention reduce the likelihood of these complications.
Prevention
Preventing Barrett’s Esophagus focuses on managing GERD and lifestyle modifications:
- Acid suppression: Use of proton pump inhibitors (PPIs) or H2 receptor blockers to control reflux.
- Weight management: Maintaining a healthy weight reduces abdominal pressure.
- Dietary modifications: Avoiding trigger foods such as spicy, fatty, or acidic foods.
- Avoid smoking and alcohol: Reduce esophageal irritation and risk of dysplasia.
- Elevate head during sleep: Helps prevent nocturnal reflux.
- Regular medical check-ups: Especially for patients with long-standing GERD to enable early endoscopic surveillance.
Korean gastroenterology clinics provide education and lifestyle guidance to prevent progression of Barrett’s Esophagus.
Treatment Options in Korea
Treatment in Korea focuses on controlling reflux, monitoring for dysplasia, and treating precancerous changes:
1. Diagnosis and Surveillance:
- Endoscopy: Visual examination of the esophagus with biopsy to detect intestinal metaplasia or dysplasia.
- Esophageal biopsy: Confirms the presence of Barrett’s tissue and grades dysplasia.
- pH monitoring: Measures acid exposure in the esophagus for reflux assessment.
2. Medical Treatments:
- Proton Pump Inhibitors (PPIs): Reduce acid production to prevent further damage.
- H2 Blockers: Alternative or adjunct to PPIs for controlling reflux.
- Lifestyle management: Diet, weight reduction, and smoking cessation programs offered by clinics.
3. Endoscopic and Surgical Treatments:
- Endoscopic mucosal resection (EMR): Removes dysplastic or early cancerous tissue.
- Radiofrequency ablation (RFA): Destroys abnormal Barrett’s tissue to prevent progression.
- Fundoplication: Surgical procedure to strengthen the lower esophageal sphincter in patients with severe reflux.
4. Follow-up and Monitoring:
- Regular endoscopic surveillance: Typically every 3–5 years for non-dysplastic BE, more frequently if dysplasia is present.
- Multidisciplinary care: Gastroenterologists, surgeons, and dietitians work together to ensure optimal outcomes.
Korean hospitals are recognized for their expertise in advanced endoscopic procedures, allowing minimally invasive management of Barrett’s Esophagus with excellent outcomes and reduced cancer risk.
In conclusion, Barrett’s Esophagus is a precancerous condition caused primarily by chronic acid reflux. Early diagnosis, lifestyle management, acid suppression, and endoscopic treatment are key to preventing complications and progression to esophageal cancer. Korea’s modern gastroenterology services provide comprehensive care, including advanced diagnostics, minimally invasive therapies, and continuous monitoring to ensure patient safety and optimal long-term health.