Overview
Barmah Forest Virus (BFV) is a mosquito-borne viral infection primarily found in Australia, but its relevance for international travelers has grown due to globalization and travel. It belongs to the Alphavirus genus and causes symptoms similar to other arboviruses, notably Ross River Virus (RRV). While BFV is rarely life-threatening, it can cause prolonged joint pain, fatigue, and discomfort that impact daily life.
In Korea, although BFV is not endemic, the country’s travel clinics and infectious disease departments are well-equipped to diagnose, prevent, and manage infections contracted abroad. Korean hospitals utilize advanced laboratory testing, supportive treatments, and preventive advice for travelers heading to endemic regions. Awareness and early intervention are crucial for minimizing symptoms and avoiding complications.
What is Barmah Forest Virus?
Barmah Forest Virus is a mosquito-transmitted virus that primarily affects humans after a bite from an infected mosquito. The virus was first identified in the Barmah Forest region of Victoria, Australia, in 1974. It is closely related to Ross River Virus, and both viruses belong to the Togaviridae family.
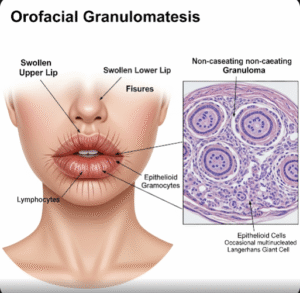
The disease caused by BFV is known as Barmah Forest Fever, which typically manifests as mild to moderate flu-like symptoms. While the infection is rarely fatal, its hallmark is polyarthritis – pain and swelling in multiple joints, often leading to significant discomfort for weeks or months. Immunity generally develops after infection, but no specific antiviral treatment exists, so management focuses on symptom relief.
Symptoms
The symptoms of Barmah Forest Virus infection usually appear 7–14 days after a mosquito bite and can include:
- Fever, often low-grade
- Rash, typically red and maculopapular, appearing on the trunk, limbs, or face
- Joint pain and swelling, particularly in the wrists, knees, ankles, and fingers
- Muscle aches and fatigue
- Headache
- Nausea or mild gastrointestinal upset in some cases
- Malaise and general discomfort
Symptoms can persist for several weeks, and in some patients, chronic joint pain or stiffness may continue for months, affecting mobility and quality of life.
Causes
The cause of BFV infection is a bite from infected mosquitoes, primarily of the Aedes and Culex genera. Mosquitoes become carriers of the virus after feeding on infected marsupials or other wildlife, which serve as natural reservoirs.
Unlike some viral infections, human-to-human transmission of BFV does not occur. Environmental factors that increase mosquito populations, such as warm temperatures, high rainfall, and stagnant water, can raise the risk of BFV outbreaks.
Risk Factors
Several factors increase the likelihood of contracting Barmah Forest Virus:
- Travel to endemic regions, particularly Australia’s coastal and forested areas.
- Exposure to mosquito-prone environments, such as wetlands, rivers, and forests.
- Lack of protective measures, such as repellents, mosquito nets, or long-sleeved clothing.
- Seasonal risk, as BFV is more prevalent during warmer months when mosquito activity peaks.
- Age and health status, with older adults or those with weakened immune systems potentially experiencing more severe symptoms.
Complications
Although complications are uncommon, BFV can lead to:
- Persistent arthritis or arthralgia, which may last for several months.
- Chronic fatigue, interfering with daily functioning and work.
- Secondary infections due to reduced mobility or scratching of mosquito bites.
- Emotional stress caused by prolonged symptoms or reduced quality of life.
Severe complications are rare, and the majority of patients recover fully with appropriate supportive care.
Prevention
Preventing Barmah Forest Virus infection focuses primarily on avoiding mosquito bites:
- Use insect repellents containing DEET, picaridin, or oil of lemon eucalyptus.
- Wear protective clothing, such as long sleeves, trousers, and socks.
- Sleep under mosquito nets in areas with high mosquito activity.
- Eliminate mosquito breeding sites, including standing water around homes or accommodation.
- Travel precautions, including avoiding peak mosquito activity hours (dawn and dusk).
For travelers from Korea to endemic regions, clinics often provide education on mosquito control, vaccination for other arboviruses if necessary, and guidance for post-travel monitoring.
Treatment Options in Korea
While there is no specific antiviral treatment for Barmah Forest Virus, Korea offers excellent supportive care for travelers or imported cases:
1. Diagnosis:
- Clinical evaluation: Assessment of fever, rash, joint pain, and travel history.
- Laboratory tests: Serology to detect BFV-specific antibodies or polymerase chain reaction (PCR) tests to confirm viral presence.
- Differential diagnosis: Important to rule out similar arboviruses such as dengue, chikungunya, and Ross River Virus.
2. Symptomatic Treatment:
- Pain and anti-inflammatory medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can relieve joint pain and swelling.
- Fever management: Paracetamol or other antipyretics help control fever.
- Hydration and rest: Adequate fluids and rest are essential for recovery.
3. Rehabilitation and Support:
- Physical therapy: Exercises to maintain joint mobility and prevent stiffness.
- Occupational therapy: Guidance for daily activities if mobility is affected.
- Psychological support: Counseling for patients experiencing prolonged fatigue or stress due to persistent symptoms.
4. Follow-up Care:
Korean hospitals provide ongoing monitoring for patients with prolonged joint pain or chronic symptoms, ensuring early detection of complications and guidance for long-term recovery. Travel medicine specialists also advise on future mosquito avoidance strategies to prevent re-infection.
In conclusion, Barmah Forest Virus is a mosquito-borne infection that can cause discomfort and prolonged joint issues, particularly in travelers from Korea visiting endemic regions. Korean medical facilities provide expert diagnosis, effective symptom management, and rehabilitation support to ensure full recovery. Preventive measures, early recognition, and supportive care are key to minimizing the impact of this viral infection.