Overview
Bacterial meningitis is a life-threatening infection that causes inflammation of the protective membranes (meninges) surrounding the brain and spinal cord. It is caused by various types of bacteria, and without rapid medical intervention, it can lead to severe neurological damage or death. The disease progresses quickly, making early recognition and treatment essential. In Korea, the healthcare system is highly equipped to handle bacterial meningitis cases with advanced diagnostic tools, specialized infectious disease teams, and modern intensive care units. Hospitals follow strict treatment protocols to provide immediate antibiotics, supportive care, and preventive measures for close contacts, ensuring effective control and recovery.
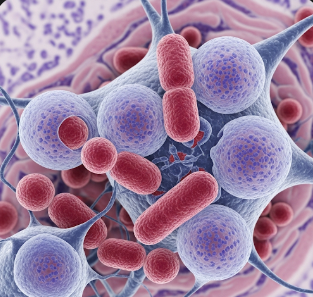
What is Bacterial Meningitis?
Bacterial meningitis occurs when bacteria enter the bloodstream and travel to the brain and spinal cord, causing inflammation of the meninges. The most common bacteria responsible include Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae type b (Hib). In newborns, Group B Streptococcus and Escherichia coli are common causes. The infection spreads rapidly and can lead to brain swelling, reduced blood flow, and damage to the nervous system. While bacterial meningitis can affect anyone, it is more common among infants, young children, teenagers, and people with weakened immune systems.
Symptoms
Bacterial meningitis symptoms can appear suddenly and worsen within hours. Common signs include:
- Severe headache
- Stiff neck
- High fever and chills
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Confusion or difficulty concentrating
- Seizures
- Sleepiness or difficulty waking up
- Skin rash (particularly in meningococcal meningitis)
In infants, symptoms may include irritability, poor feeding, unusual crying, and a bulging soft spot (fontanel) on the head.
Causes
Bacterial meningitis is caused by the invasion of bacteria into the bloodstream and then into the meninges. Common sources and transmission routes include:
- Respiratory droplets – spread through coughing, sneezing, or close contact with an infected person
- Direct spread from infections – such as sinusitis, ear infections, or pneumonia
- Bloodstream infections – where bacteria circulate and reach the brain
- Birth-related transmission – in newborns, bacteria can be passed from mother to baby during delivery
- Head injuries or surgeries – that allow bacteria to enter the cerebrospinal fluid
Risk Factors
Certain factors increase the likelihood of developing bacterial meningitis:
- Being under the age of 5 or between 16–25 years
- Living in crowded environments like dormitories or military barracks
- Weakened immune system from HIV, cancer, or immunosuppressive drugs
- Chronic illnesses such as diabetes or kidney disease
- Recent head trauma or neurosurgery
- Lack of vaccination against meningitis-causing bacteria
Complications
If untreated or treated too late, bacterial meningitis can lead to serious, long-term health issues, including:
- Hearing loss (partial or complete)
- Memory problems and learning disabilities
- Brain damage and cognitive impairment
- Seizure disorders
- Hydrocephalus (fluid buildup in the brain)
- Amputations due to severe blood clotting in meningococcal cases
- Death, especially if diagnosis and treatment are delayed
Prevention
Preventing bacterial meningitis is possible through a combination of vaccination, hygiene, and prompt treatment of related infections:
- Vaccination – Korea offers vaccines against major bacteria causing meningitis, such as Hib, pneumococcal, and meningococcal vaccines
- Good hygiene practices – regular handwashing and avoiding sharing utensils or drinks
- Prompt treatment of infections – such as ear infections, sinusitis, and pneumonia
- Prophylactic antibiotics – for people in close contact with a meningitis patient, as recommended by doctors
- Immune health maintenance – through proper nutrition, exercise, and sleep
Treatment Options in Korea
1. Diagnosis
Quick and accurate diagnosis is crucial for bacterial meningitis. Korean hospitals use advanced diagnostic methods, including:
- Lumbar puncture (spinal tap) – to examine cerebrospinal fluid for bacteria, white blood cells, and protein levels
- Blood cultures – to detect bacteria in the bloodstream
- Polymerase chain reaction (PCR) testing – to identify bacterial DNA quickly
- Brain imaging (CT or MRI) – to detect swelling or complications before a spinal tap if needed
2. Medical Treatments
- Immediate intravenous antibiotics – started as soon as bacterial meningitis is suspected, even before test results are complete
- Corticosteroids – to reduce inflammation and lower the risk of hearing loss or brain damage
- Intravenous fluids – to maintain hydration and support blood pressure
- Anticonvulsants – to control seizures if they occur
- Oxygen therapy – if breathing is affected
3. Supportive Care in Hospitals
Korea’s major medical centers have advanced intensive care units (ICUs) that provide:
- Continuous neurological monitoring
- Ventilator support if needed
- Strict infection control measures to prevent spread
4. Rehabilitation and Follow-Up
After acute treatment, Korean hospitals offer rehabilitation programs for patients who experience after-effects:
- Hearing rehabilitation – with hearing aids or cochlear implants
- Physical therapy – to improve strength and mobility
- Speech and occupational therapy – for cognitive or language recovery
- Psychological counseling – for emotional support after severe illness
5. Medical Tourism and Global Expertise
South Korea is a top destination for complex infectious disease treatment due to its rapid-response medical system and advanced hospital infrastructure. International patients benefit from:
- Multilingual medical teams
- State-of-the-art laboratories for rapid bacterial detection
- Private patient rooms with advanced infection prevention technology
- Access to world-class neurologists and infectious disease specialists