Overview
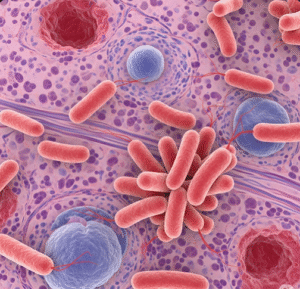
Autoimmune Pancreatitis (AIP) is a rare form of chronic pancreatitis caused by the body’s immune system attacking the pancreas, leading to inflammation and fibrosis. It can mimic pancreatic cancer but typically responds well to steroid treatment. Early diagnosis is important to avoid unnecessary surgery and manage symptoms effectively.
What is Autoimmune Pancreatitis?
AIP is an immune-mediated disease characterized by swelling of the pancreas and narrowing of the pancreatic duct due to inflammation. It is classified into two types: Type 1 (associated with IgG4-related disease) and Type 2 (idiopathic duct-centric pancreatitis). The disease can cause obstructive jaundice and pancreatic dysfunction.
Symptoms
- Painless jaundice (yellowing of the skin and eyes)
- Abdominal pain or discomfort
- Weight loss
- Fatigue
- Diabetes or worsening glucose control
- Pancreatic insufficiency (malabsorption, diarrhea)
- Occasionally, symptoms related to other organs if IgG4 disease is systemic
Causes
The exact cause is unknown, but AIP results from an abnormal autoimmune reaction leading to inflammation and fibrosis of pancreatic tissue. Type 1 AIP is often part of systemic IgG4-related disease affecting multiple organs.
Risk Factors
- Middle-aged and older adults (typically 50-70 years)
- Male gender (more common in men)
- History of other autoimmune diseases
- Elevated serum IgG4 levels (Type 1 AIP)
Complications
- Obstruction of bile ducts causing cholangitis
- Pancreatic insufficiency leading to malnutrition
- Development of diabetes mellitus
- Misdiagnosis leading to unnecessary pancreatic surgery
- Recurrence of inflammation requiring repeated treatment
Prevention
- No known prevention due to autoimmune nature
- Early diagnosis and treatment to prevent complications
- Regular follow-up after treatment to monitor for relapse
Treatment Options in Korea
South Korea offers specialized gastroenterology and immunology services with advanced diagnostic tools and effective treatment protocols for AIP.
- Diagnosis
- Blood tests including serum IgG4 levels
- Imaging studies: CT scan, MRI, and Endoscopic Ultrasound (EUS)
- Pancreatic biopsy in uncertain cases
- Differential diagnosis to exclude pancreatic cancer
- Medication
- Corticosteroids: First-line treatment to reduce inflammation and induce remission
- Immunosuppressants: Azathioprine or mycophenolate mofetil for maintenance or steroid-refractory cases
- Supportive care: Enzyme replacement therapy for pancreatic insufficiency
- Monitoring and Follow-Up
- Regular imaging and blood tests to detect relapse
- Management of diabetes or other complications