Overview
Aggressive Periodontitis is a severe and rapidly progressing form of gum disease that primarily affects young individuals. Unlike chronic periodontitis, which develops slowly, aggressive periodontitis causes significant destruction of the supporting structures of the teeth — including the bone — in a relatively short time. Early diagnosis and treatment are critical to prevent tooth loss.
What is Aggressive Periodontitis?
Aggressive periodontitis is a type of periodontal disease characterized by rapid loss of gum attachment and bone, often occurring in patients who are otherwise healthy. It may affect a few teeth (localized) or many teeth (generalized) and is often linked to genetic factors and immune system dysfunction.
It is distinct from other gum diseases because of its early onset, typically during adolescence or early adulthood, and the speed of progression.
Symptoms
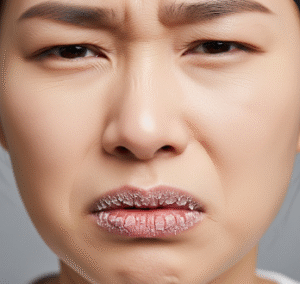
Aggressive periodontitis may present with subtle or no symptoms in early stages, making regular dental checkups essential. When symptoms do appear, they can include:
- Deep gum pockets
- Gum recession
- Loose or shifting teeth
- Bleeding gums during brushing or flossing
- Bad breath (halitosis)
- Pain when chewing (in advanced cases)
- Pus between teeth and gums
Causes
The primary cause of aggressive periodontitis is bacterial infection, especially involving Aggregatibacter actinomycetemcomitans and other periodontal pathogens. However, what distinguishes this condition is the exaggerated immune response that leads to rapid tissue destruction.
Contributing causes include:
- Genetic predisposition
- Impaired neutrophil function (white blood cells)
- Plaque and tartar buildup (although destruction is more severe than expected for the level of buildup)
Risk Factors
Several factors increase the risk of developing aggressive periodontitis:
- Family history of periodontal disease
- Teenage or young adult age group
- Poor oral hygiene
- Smoking
- Weakened immune system
- Hormonal changes, such as during puberty
- Stress, which may affect immune function
Complications
If untreated, aggressive periodontitis can lead to:
- Tooth mobility and eventual tooth loss
- Spread of infection to surrounding bone
- Aesthetic concerns due to gum recession
- Difficulty chewing or speaking
- Systemic health issues, as periodontitis may increase the risk of heart disease, diabetes, and respiratory conditions
Prevention
Preventive strategies focus on maintaining good oral health and early detection:
- Brush teeth twice daily with fluoride toothpaste
- Floss daily to remove plaque between teeth
- Visit the dentist regularly for cleanings and checkups
- Avoid smoking
- Manage underlying conditions, such as diabetes
- Prompt treatment of early gum disease signs
If there’s a family history, regular periodontal evaluation is especially important.
Treatment Options Korea
Treatment of aggressive periodontitis aims to control infection, halt progression, and restore lost support:
- Professional Cleaning (Scaling and Root Planing)
Removes plaque and tartar beneath the gumline. - Antibiotic Therapy
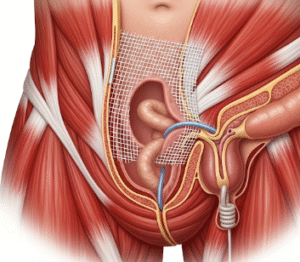
Systemic or local antibiotics (e.g., doxycycline, metronidazole) help control bacterial infection. - Surgical Intervention
May include flap surgery, bone grafting, or guided tissue regeneration to repair damaged bone and gums. - Ongoing Periodontal Maintenance
Regular follow-up cleanings every 3–4 months to prevent recurrence. - Lifestyle Modifications
Smoking cessation and improved oral hygiene are essential to long-term success.
Early and aggressive intervention greatly improves the prognosis for individuals with aggressive periodontitis.