Overview
Acute pancreatitis is a sudden inflammation of the pancreas that can range from mild discomfort to a life-threatening condition. It often begins abruptly and can resolve with proper treatment, but in severe cases, it may lead to complications such as organ failure or infection. Early diagnosis and appropriate care are essential to reduce risk and promote recovery.
What is Acute Pancreatitis?
Acute pancreatitis is an inflammatory condition of the pancreas that occurs suddenly and typically lasts a few days. The pancreas is an organ behind the stomach that produces enzymes to aid digestion and hormones to regulate blood sugar. In acute pancreatitis, these digestive enzymes become active inside the pancreas, causing the organ to digest itself and resulting in inflammation.
Symptoms
Common signs and symptoms of acute pancreatitis include:
- Severe upper abdominal pain (may radiate to the back)
- Abdominal tenderness and swelling
- Nausea and vomiting
- Fever
- Rapid pulse
- Loss of appetite
- Fatigue
- Bloating or indigestion
In severe cases:
- Difficulty breathing
- Low blood pressure
- Confusion or dizziness
Causes
Several factors can trigger acute pancreatitis, including:
- Gallstones (most common cause)
- Excessive alcohol consumption
- High triglyceride levels
- Certain medications (e.g., corticosteroids, diuretics)
- Infections
- Abdominal trauma
- Pancreatic cancer or tumors
- Genetic disorders
- Autoimmune diseases
- Endoscopic procedures (ERCP)
Risk Factors
People are at higher risk of developing acute pancreatitis if they have:
- Gallbladder disease (especially gallstones)
- Heavy alcohol use
- A family history of pancreatitis
- Obesity
- High triglyceride or calcium levels
- Smoking
- Diabetes
- Use of certain prescription medications
Complications
Though many cases resolve without issues, acute pancreatitis can lead to:
- Pancreatic necrosis (tissue death)
- Infections within the pancreas
- Pseudocysts (fluid-filled sacs)
- Breathing problems
- Kidney failure
- Malnutrition
- Systemic inflammatory response syndrome (SIRS)
- Multiple organ failure
- Chronic pancreatitis if attacks recur
Prevention
Preventing acute pancreatitis involves addressing modifiable risk factors:
- Avoid heavy alcohol consumption
- Maintain a healthy weight
- Treat gallstones early (cholecystectomy if necessary)
- Manage triglyceride and cholesterol levels
- Avoid smoking
- Monitor medications that may irritate the pancreas
- Control diabetes and other chronic conditions
Treatment Options Korea
1. Hospital Admission and Monitoring
- Most patients with moderate to severe pancreatitis are hospitalized
- Continuous monitoring of:
- Vital signs, electrolytes, renal function, and amylase/lipase levels
- CT or ultrasound to assess pancreatic inflammation and complications
- Treated in gastroenterology, internal medicine, or ICU for severe cases
2. Initial Supportive Management
- NPO (nothing by mouth) to rest the pancreas
- IV fluid resuscitation is the mainstay (e.g., lactated Ringer’s solution)
- Pain control using IV opioids or NSAIDs
3. Nutritional Support
- Begin oral feeding as soon as tolerated (clear liquid → low-fat diet)
- In severe cases, enteral feeding via nasojejunal tube preferred over TPN (IV nutrition)
4. Treatment of Underlying Cause
- Gallstone pancreatitis:
- May require ERCP (Endoscopic Retrograde Cholangiopancreatography) to remove bile duct stones
- Cholecystectomy (gallbladder removal) typically performed before discharge
- Alcohol-induced pancreatitis:
- Managed with abstinence support and counseling
- Referral to alcohol cessation programs
5. Antibiotics (Only If Infection Confirmed)
- Not routinely used unless:
- Suspected or confirmed infected pancreatic necrosis
- Associated cholangitis or sepsis
- Used under guidance of infectious disease specialists
6. Management of Complications
- Pancreatic pseudocysts or abscesses:
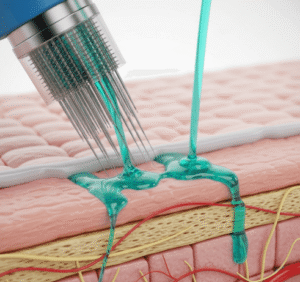
- May require drainage (percutaneous or endoscopic)
- Necrotizing pancreatitis:
- Managed with step-up approach: minimally invasive drainage → surgery if needed
- Available at specialized gastroenterology centers in Korea
7. Follow-Up and Prevention
- Identify and manage risk factors: gallstones, alcohol, hypertriglyceridemia
- Lifestyle modification, fat-controlled diet, and long-term GI follow-up
- Prevent recurrence through education and specialist care