Overview
Actinomycosis is a rare but chronic bacterial infection caused primarily by Actinomyces species — bacteria that normally live harmlessly in the mouth, throat, and gastrointestinal tract. When the mucosal barrier is broken due to trauma, surgery, or infection, these bacteria can invade deeper tissues and cause painful abscesses, swelling, and tissue damage.
This condition progresses slowly but can become severe if untreated. It’s most common in the face and neck, but can also occur in the chest, abdomen, or pelvis. Although it may mimic tumors or other infections, early diagnosis and long-term antibiotic treatment can lead to full recovery.
What is Actinomycosis?
Actinomycosis is a chronic granulomatous infection caused by filamentous, anaerobic bacteria (most commonly Actinomyces israelii). It typically results in abscess formation, tissue fibrosis, and draining sinus tracts. The infection is not contagious and tends to develop over weeks to months.
Common forms include:
- Cervicofacial actinomycosis (most common)
- Thoracic actinomycosis
- Abdominal actinomycosis
- Pelvic actinomycosis (especially in women with IUDs)
Symptoms
Symptoms vary depending on the location but may include:
Cervicofacial Actinomycosis:
- Painful swelling or lump on the jaw or neck
- Draining sores or abscesses
- “Lumpy jaw” appearance
- Fever and malaise
- Difficulty opening the mouth (trismus)
Thoracic Actinomycosis:
- Chronic cough
- Chest pain
- Fever
- Weight loss
- Pulmonary masses mimicking cancer
Abdominal Actinomycosis:
- Abdominal pain
- Fever
- Nausea or vomiting
- Abdominal mass or abscess
- Fistulas or sinus tracts
Pelvic Actinomycosis:
- Lower abdominal or pelvic pain
- Vaginal discharge
- Possible connection to long-term IUD use
Causes
The infection is caused by:
- Actinomyces bacteria, primarily Actinomyces israelii, which are part of normal flora in the mouth and gut.
They become pathogenic when:
- The mucosal barrier is breached due to:
- Dental infections or oral trauma
- Abdominal surgeries or bowel perforation
- Long-term intrauterine device (IUD) use
- Lung aspiration or infections
Risk Factors
You are more likely to develop actinomycosis if you:
- Have poor dental hygiene or untreated dental infections
- Recently had oral or abdominal surgery
- Suffer from bowel diseases like diverticulitis or appendicitis
- Use an IUD for long durations (especially over 3 years)
- Are immunocompromised (e.g., cancer, diabetes, HIV)
- Have had trauma or injury to mucous membranes
Complications
If not treated promptly, actinomycosis can lead to:
- Chronic abscesses
- Sinus tract formation (channels that drain pus to the skin)
- Fibrosis and scarring
- Spread of infection to bones or organs
- Misdiagnosis as cancer or tuberculosis
- Rarely, sepsis or systemic infection
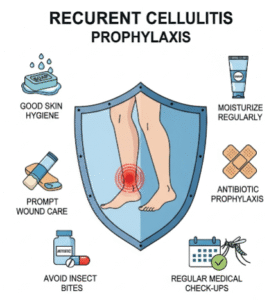
Prevention
Although actinomycosis cannot always be prevented, you can reduce risk by:
- Maintaining good oral hygiene
- Seeking prompt dental care for infections or abscesses
- Avoiding prolonged use of intrauterine devices (IUDs)
- Treating gastrointestinal conditions that may cause mucosal injury
- Avoiding trauma to the mouth or GI tract during procedures
Treatment Options Korea
1. Long-term Antibiotic Therapy
- First-line treatment is prolonged use of high-dose penicillin
- Typical duration:
- IV penicillin G for 2–6 weeks
- Followed by oral penicillin or amoxicillin for 6–12 months
- Alternatives (for penicillin allergy): doxycycline, erythromycin, or clindamycin
2. Surgical Intervention
- Used to drain abscesses, remove necrotic tissue, or excise masses
- Especially necessary in cervicofacial, thoracic, or abdominal forms
- Performed in general surgery or ENT units at Korean hospitals
3. Imaging and Biopsy
- CT or MRI scans to assess lesion extent and rule out malignancy
- Biopsy or culture often required to confirm diagnosis (due to mimicry of tumors)
4. Supportive Care
- Pain management, nutritional support, and wound care
- Monitoring for recurrence or fistula formation
5. Follow-Up and Monitoring
- Regular follow-ups to ensure complete resolution
- Adjust duration of therapy based on clinical and imaging response