Overview
Achalasia is a rare disorder of the esophagus, the tube that carries food from the mouth to the stomach. It occurs when the lower esophageal sphincter (LES) — a ring of muscle at the bottom of the esophagus — fails to relax properly, making it difficult for food and liquid to pass into the stomach. This condition gradually worsens over time and can significantly affect a person’s ability to eat, drink, and maintain a healthy weight if not treated.
What is Achalasia?
Achalasia is a chronic esophageal motility disorder caused by nerve damage in the esophagus. It primarily affects the ability of the esophagus to move food toward the stomach and the LES to open during swallowing. As a result, food and liquids become trapped in the esophagus, leading to discomfort, regurgitation, and sometimes aspiration.
Achalasia is considered a primary motility disorder and is not caused by another disease. However, there are secondary forms of achalasia that may result from other conditions like cancer or infections.
Symptoms
Symptoms often develop gradually and worsen over time:
- Difficulty swallowing (dysphagia), especially for solids and later for liquids
- Regurgitation of undigested food
- Chest pain or discomfort (often mistaken for heart pain)
- Weight loss
- Heartburn or acid reflux-like symptoms
- Coughing or choking, especially at night
- Hoarseness or sore throat
- Bad breath (halitosis)
Causes
The exact cause of achalasia is unknown in most cases. It is believed to result from:
- Degeneration of nerves in the esophageal wall, particularly the myenteric plexus
- Autoimmune response, where the body attacks its own nerve cells
- Genetic factors (in rare familial cases)
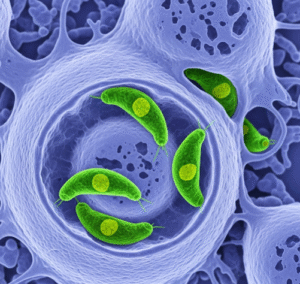
- Infections, such as Chagas disease (in South America, caused by Trypanosoma cruzi)
In rare cases, achalasia can be secondary to cancers that affect the nerves of the esophagus (pseudoachalasia).
Risk Factors
- Middle-aged and older adults (most cases occur between ages 25–60)
- Family history of achalasia (rare)
- Autoimmune conditions
- Chagas disease (in endemic regions)
Complications
If untreated, achalasia can lead to serious issues, including:
- Significant weight loss and malnutrition
- Aspiration pneumonia (inhaling food or liquid into the lungs)
- Esophageal dilation (widening)
- Esophageal ulcers or inflammation
- Esophageal perforation (in rare cases)
- Increased risk of esophageal cancer, especially squamous cell carcinoma
Prevention
There is currently no known way to prevent idiopathic (primary) achalasia. However, you can reduce complications through:
- Early diagnosis and treatment
- Regular follow-up care
- Maintaining a soft or liquid diet during flare-ups
- Proper swallowing techniques and upright posture during/after meals
For Chagas disease-related achalasia, preventing parasite transmission is key in endemic areas.
Treatment Options for Achalasia in Korea
1. Medications (for mild symptoms)
- Calcium channel blockers or nitrates
- Reduce lower esophageal sphincter (LES) pressure
- Limited long-term effect
2. Pneumatic Balloon Dilation
- Endoscopic stretching of LES with a balloon
- Common first-line procedure in Korean hospitals
- May require repeat sessions
3. Botulinum Toxin (Botox) Injection
- Injected into LES during endoscopy
- Temporary relief (lasts a few months)
- Used in elderly or high-risk patients
4. Laparoscopic Heller Myotomy (LHM)
- Surgical cutting of LES muscle
- Often combined with anti-reflux procedure
- Available in tertiary hospitals like Asan or Severance
5. Peroral Endoscopic Myotomy (POEM)
- Minimally invasive endoscopic surgery
- Increasingly preferred in Korea
- Short recovery, effective long-term