Overview
An Abdominal Aortic Aneurysm (AAA) is a potentially life-threatening condition where the lower part of the aorta—the major blood vessel supplying blood from the heart to the body—becomes enlarged or bulges outward. This dilation typically occurs in the abdominal region, below the chest. While small aneurysms may be harmless and symptomless, larger ones carry a serious risk of sudden rupture, leading to massive internal bleeding and possibly death if not treated immediately.
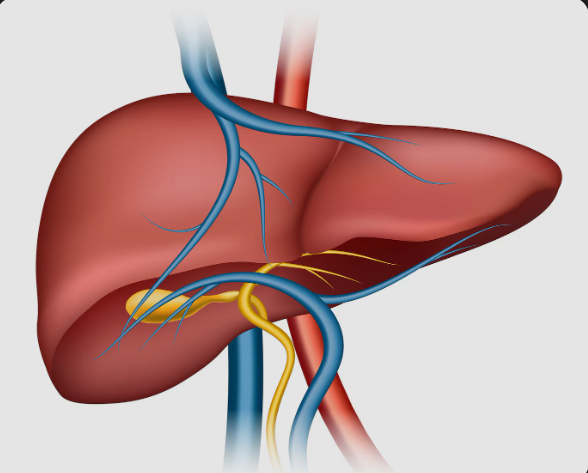
What Is an Abdominal Aortic Aneurysm?
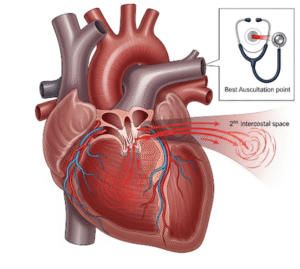
The aorta is the largest artery in the body, responsible for distributing oxygen-rich blood from the heart to all major organs. An abdominal aortic aneurysm occurs when the abdominal portion of this artery weakens and balloons outward.
AAAs often grow slowly and remain asymptomatic. However, once the aneurysm reaches a certain size, the risk of rupture increases significantly. Prompt diagnosis and treatment are critical to preventing serious complications.
Symptoms
Many individuals with AAA do not exhibit any symptoms until the aneurysm enlarges or ruptures. When present, symptoms may include:
- A deep, persistent pain in the abdomen or lower back
- A pulsating sensation near the belly button (navel)
- Sudden, intense abdominal or back pain
- Low blood pressure, rapid heart rate, fainting (indicating possible rupture)
⚠️ Emergency Warning: A ruptured AAA is a medical emergency requiring immediate attention to prevent death.
Causes
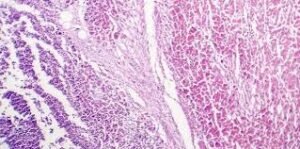
The exact cause of an abdominal aortic aneurysm is not always clear, but several factors may contribute to the weakening of the aortic wall:
- Atherosclerosis (buildup of plaque inside arteries)
- Chronic high blood pressure (hypertension)
- Smoking (a major risk factor)
- Infections or inflammatory diseases of blood vessels
- Genetic disorders affecting connective tissue (e.g., Marfan syndrome)
- Physical trauma to the abdomen
Risk Factors
You’re more likely to develop an AAA if you have one or more of the following risk factors:
- Age over 65
- Male gender (significantly higher prevalence in men)
- History of smoking
- Family history of aneurysms
- High blood pressure and cholesterol
- Obesity
- Atherosclerosis
- Chronic obstructive pulmonary disease (COPD)
- Inflammatory vascular conditions
Complications
The most serious and immediate complication of an AAA is rupture, which can lead to:
- Massive internal bleeding
- Hypovolemic shock
- Organ failure
- Sudden death
Other potential complications include:
- Thrombosis (blood clot formation) inside the aneurysm
- Reduced blood flow to legs or abdominal organs
- Compression of surrounding structures, such as nerves or ureters
Prevention
While not all abdominal aortic aneurysms can be prevented, risk reduction is possible through healthy lifestyle choices and early screening:
- Quit smoking (the most effective preventive measure)
- Control blood pressure and cholesterol levels
- Exercise regularly
- Eat a heart-healthy, low-sodium diet
- Maintain a healthy weight
- Manage diabetes and chronic illnesses
- Undergo routine screening if you are male and over 65, or have a family history of aneurysms
Treatment Options in Korea
South Korea offers advanced medical care for AAA, ranging from early detection to life-saving surgical interventions. Key treatment options include:
1. Screening and Diagnosis
- Abdominal ultrasound: Widely used for routine screening
- CT angiography or MRI: For detailed imaging of the aneurysm
- Recommended screening for men aged 65–75 who have ever smoked
2. Monitoring (Watchful Waiting)
- Small AAAs (<5.5 cm in men, <5.0 cm in women) may be monitored with regular imaging
- Lifestyle modifications and blood pressure control emphasized
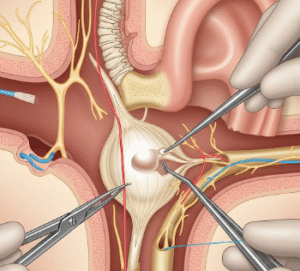
3. Surgical Treatment
- Endovascular Aneurysm Repair (EVAR):
- Minimally invasive
- Involves inserting a stent graft through blood vessels to reinforce the aorta
- Shorter hospital stay and quicker recovery
- Open Surgical Repair:
- Involves open abdominal surgery to replace the weakened section of the aorta
- Typically used for younger or fit patients, or when EVAR is not suitable
4. Postoperative and Long-Term Care
- Rehabilitation support in major hospitals
- Continued imaging and monitoring for graft complications
- Lifestyle counseling and chronic disease management