Overview
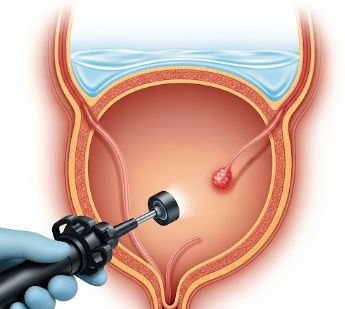
Cystoscopy is a medical procedure that allows direct visualization of the urinary bladder and urethra using a specialized instrument called a cystoscope. This procedure is essential for diagnosing, monitoring, and treating urinary tract conditions.
Importance of cystoscopy:
- Provides accurate assessment of the bladder lining and urethra.
- Detects tumors, stones, inflammation, strictures, and infections.
- Guides biopsies, stone removal, and surgical interventions.
- Enables early diagnosis of urinary tract cancers, especially bladder cancer.
In South Korea, cystoscopy is routinely performed in urology departments of hospitals, specialized clinics, and teaching hospitals, using advanced flexible and rigid cystoscopes for patient comfort and precise imaging.
Why It’s Done
Cystoscopy is performed to investigate urinary tract symptoms, monitor conditions, and guide treatment.
Common indications include:
- ➤ Hematuria (blood in urine), both visible and microscopic.
- ➤ Recurrent urinary tract infections (UTIs).
- ➤ Lower urinary tract symptoms: Frequent urination, urgency, or pain.
- ➤ Bladder tumors or suspicious lesions detected on imaging.
- ➤ Urinary obstruction: Evaluation of strictures, stones, or enlarged prostate.
- ➤ Follow-up after bladder surgery or treatment for cancer.
Benefits for patients:
- ✔️ Direct visualization allows accurate diagnosis.
- ✔️ Minimally invasive approach compared to open surgery.
- ✔️ Enables biopsy and therapeutic interventions in the same session.
- ✔️ Reduces the need for repeated imaging or exploratory procedures.
- ✔️ Supports early detection of malignancies, improving outcomes.
Alternatives
While cystoscopy provides a direct view, other diagnostic or monitoring options may be considered:
- ➤ Ultrasound: Non-invasive imaging of the kidneys, ureters, and bladder.
- ➤ CT urography: Detailed imaging for stones, tumors, and obstruction.
- ➤ MRI of the urinary tract: Useful for soft tissue characterization.
- ➤ Urine cytology: Microscopic examination of urine for abnormal cells.
- ➤ Intravenous pyelogram (IVP): X-ray imaging of urinary tract with contrast.
Key point: Cystoscopy is the gold standard for bladder evaluation, particularly when lesions, tumors, or unexplained hematuria are suspected.
Preparation
Proper preparation ensures safety, patient comfort, and accurate results.
Steps include:
- ✅ Medical history: Discuss allergies, medications, anticoagulants, and prior urologic procedures.
- ✅ Urine test: Screening for infection; antibiotics may be prescribed if necessary.
- ✅ Hydration: Drink water to ensure a moderately full bladder for optimal visualization.
- ✅ Fasting: Usually not required for outpatient cystoscopy, but may be needed if sedation is planned.
- ✅ Consent: Understand procedure, risks, and alternatives.
- ✅ Arrange transportation: Required if sedation or anesthesia is used.
Important: Preparation reduces infection risk, improves patient comfort, and ensures procedure effectiveness.
How It’s Done
Cystoscopy can be performed using a rigid or flexible cystoscope, depending on clinical need and patient comfort.
Procedure steps:
- Patient positioning: Usually lying on the back with legs apart; specialized table for males and females.
- Anesthesia: Local anesthetic gel for urethra; sedation or general anesthesia may be used in selected cases.
- Cystoscope insertion: The cystoscope is gently inserted through the urethra into the bladder.
- Bladder examination: Saline is instilled to expand the bladder, allowing clear visualization of the bladder wall and ureteric openings.
- Interventions (if required):
- Biopsy of suspicious tissue
- Stone removal
- Removal of small tumors or foreign bodies
- Placement of stents or catheters
- Completion: Cystoscope is carefully withdrawn; patient may feel temporary burning or urgency.
Key point: Flexible cystoscopy is more comfortable and can often be performed in outpatient settings, while rigid cystoscopy allows therapeutic procedures.
Recovery & Post-Care
After cystoscopy, most patients recover quickly, especially after flexible cystoscopy without sedation.
Immediate post-procedure care:
- ✅ Mild burning during urination or slight blood in urine is common.
- ✅ Drink plenty of fluids to flush the urinary tract.
- ✅ Rest for the remainder of the day if sedation was used.
Follow-up:
- Discuss biopsy results if tissue was collected.
- Schedule additional cystoscopy for monitoring bladder cancer or other chronic conditions.
- Report persistent pain, fever, or heavy bleeding to a physician immediately.
Long-term outcomes:
- Enables early detection and treatment of urinary tract abnormalities.
- Reduces the need for more invasive diagnostic procedures.
- Supports monitoring of chronic conditions, improving patient outcomes.
Important: Post-procedure hydration and hygiene reduce infection risk.
Possible Complications / Risks
Cystoscopy is generally safe, but potential risks include:
- ⚠️ Urinary tract infection (UTI): Most common complication; antibiotics may be prescribed.
- ⚠️ Bleeding: Minor hematuria is common; significant bleeding is rare.
- ⚠️ Pain or discomfort: Temporary burning, urgency, or pelvic discomfort.
- ⚠️ Urethral injury or stricture: Rare, more likely with rigid cystoscopy.
- ⚠️ Allergic reactions: Rare reactions to local anesthetic gel or contrast if used.
In South Korea, urology departments follow strict sterile protocols, anesthesia safety measures, and post-procedure monitoring to minimize risks.
Treatment Options / Clinical Relevance in Korea
Cystoscopy is a widely accessible and essential diagnostic tool in South Korea, performed in hospitals, specialized urology clinics, and teaching hospitals.
Key features:
- 🏥 Flexible cystoscopy for outpatient evaluation of hematuria, infections, and lower urinary tract symptoms.
- 🏥 Rigid cystoscopy for therapeutic interventions such as stone removal, biopsy, and tumor excision.
- 🏥 High-resolution cystoscopes with video capability for detailed visualization and documentation.
- 🏥 Integration with digital imaging systems allows recording, monitoring, and teleconsultation.
- 🏥 Specialized programs for bladder cancer surveillance and chronic urinary tract monitoring.
Highlights in Korea:
- ✔️ Early detection of bladder cancer and urinary tract lesions improves survival rates.
- ✔️ Outpatient flexible cystoscopy enhances patient convenience and comfort.
- ✔️ Therapeutic cystoscopy reduces need for open surgery.
- ✔️ Integration with advanced imaging and lab tests ensures comprehensive urological care.
- ✔️ Widespread access across hospitals ensures timely diagnosis and intervention.
Highlights
- ➤ Cystoscopy provides direct visualization of the bladder and urethra.
- ➤ Indicated for hematuria, recurrent UTIs, urinary obstruction, bladder tumors, and follow-up after urologic procedures.
- ➤ Alternatives include ultrasound, CT urography, MRI, urine cytology, and IVP.
- ➤ Preparation involves medical history, urine test, hydration, consent, and possibly fasting.
- ➤ Procedure uses rigid or flexible cystoscope, local anesthesia, saline bladder filling, and allows biopsy or stone removal if needed.
- ➤ Post-procedure care includes hydration, monitoring for infection, and follow-up appointments.
- ➤ South Korea offers advanced cystoscopy with high-resolution scopes, outpatient options, and integrated digital monitoring for optimal urological care.