Overview
Croup is a common childhood respiratory illness characterized by swelling of the upper airways, leading to a distinctive barking cough and hoarseness. It is usually caused by viral infections and primarily affects children under 5 years of age. In Korea, pediatric care and hospital facilities are well-equipped to manage croup, with early diagnosis and effective treatments available.
What is Croup?
Croup (also called laryngotracheobronchitis) is an infection of the upper airway, including the larynx and trachea, which causes narrowing and breathing difficulties. It is most often viral in origin, but in rare cases, bacterial infections can also cause croup. It spreads through respiratory droplets, and symptoms typically worsen at night.
Symptoms
- Barking cough (like a seal)
- Hoarseness
- Stridor (high-pitched breathing sound, especially during inhalation)
- Fever (usually mild)
- Runny nose and cold-like symptoms before cough starts
- Difficulty breathing (in severe cases)
- Irritability or fatigue
Causes
- Viral infections (most common: parainfluenza virus, influenza, adenovirus, respiratory syncytial virus)
- Less common: bacterial infections
- Allergic reactions or irritants can sometimes mimic croup-like symptoms
Risk Factors
- Children between 6 months and 5 years are most at risk
- Contact with infected individuals
- Seasonal peaks (late fall and early winter in Korea)
- History of respiratory issues or allergies
Complications
- Severe airway obstruction requiring hospitalization
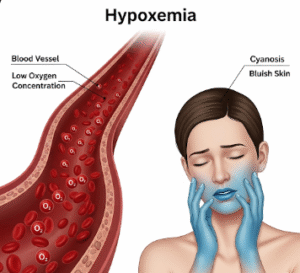
- Respiratory distress or hypoxia (low oxygen)
- Rarely, secondary bacterial infections (tracheitis, pneumonia)
- Recurrent episodes in some children
Prevention
- Good hygiene: frequent handwashing, mask use during respiratory infections
- Limiting exposure to sick individuals
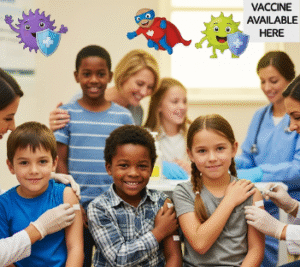
- Annual flu vaccination (recommended for children in Korea)
- Avoiding exposure to smoke or air pollutants
Treatment Options in Korea
Korean healthcare facilities provide comprehensive care for croup, with pediatricians and emergency departments well-prepared to handle both mild and severe cases.
- Diagnosis
- Based on clinical symptoms and physical examination
- Oxygen saturation monitoring in moderate to severe cases
- Rarely, imaging (neck X-ray) to rule out other causes
- Medical Treatment
- Mild cases: supportive care at home (humidified air, fluids, rest)
- Moderate to severe cases: oral or nebulized corticosteroids (e.g., dexamethasone)
- Nebulized epinephrine in emergency situations for airway swelling
- Oxygen therapy if breathing difficulty is significant
- Follow-up and Support
- Most children recover fully within 3–5 days
- Parents are educated on signs of breathing distress
- Follow-up with pediatrician if symptoms worsen or recur