Overview
Mastectomy is a surgical procedure to remove one or both breasts, partially or completely, typically to treat or prevent breast cancer. It may also be indicated for severe benign breast disease or high-risk individuals with a strong family history of breast cancer.
In Korea, mastectomy is performed by experienced breast surgeons using advanced surgical and reconstructive techniques, ensuring optimal oncologic outcomes, minimal scarring, and, when appropriate, immediate or delayed breast reconstruction.
Highlights:
- ✅ Removes cancerous or high-risk breast tissue
- ✅ Can be combined with breast reconstruction
- ✅ Minimally invasive options for certain cases
- ✅ Reduces recurrence risk and improves survival in selected patients
What is Mastectomy?
Mastectomy involves removal of breast tissue, which may include:
- Simple (total) mastectomy: Removal of the entire breast without lymph nodes
- Modified radical mastectomy: Removal of the breast and nearby lymph nodes
- Radical mastectomy: Removal of breast, chest wall muscles, and lymph nodes (rarely done today)
- Skin-sparing or nipple-sparing mastectomy: Preserves skin or nipple for reconstruction
Indications include:
- Breast cancer (invasive or ductal carcinoma in situ)
- High genetic risk (BRCA mutations)
- Recurrent breast infections or benign tumors (rare)
Important: The type of mastectomy depends on cancer type, stage, patient preference, and reconstructive considerations.
What are the benefits?
- Cancer treatment: Removes malignant tissue to reduce risk of recurrence
- Prevention: High-risk patients can significantly lower cancer risk
- Reconstruction options: Allows immediate or delayed reconstruction for cosmetic restoration
- Improved survival: Effective component of comprehensive breast cancer management
Key benefits highlighted:
- ⚡ Removes entire affected breast tissue
- ⚡ Minimizes cancer recurrence risk
- ⚡ Preserves possibility for reconstruction
- ⚡ Can be combined with other treatments like chemotherapy or radiotherapy
Procedure Details
1) How should I prepare for Mastectomy?
- Preoperative evaluation: Mammography, ultrasound, MRI, blood tests, ECG, and imaging to assess tumor and lymph nodes
- Medication review: Stop blood thinners or medications as advised
- Fasting: 8–12 hours before surgery
- Consent and counseling: Discuss type of mastectomy, risks, reconstruction options, and recovery expectations
- Lifestyle preparation: Arrange for postoperative support, transportation, and wound care
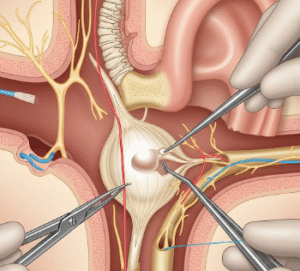
2) What happens during Mastectomy?
- Anesthesia: General anesthesia administered
- Incision: Surgeon removes breast tissue according to chosen procedure
- Lymph node removal: Performed if cancer spread assessment is required
- Closure: Incision closed with sutures; drains may be placed to prevent fluid accumulation
- Optional reconstruction: Immediate reconstruction using implants or autologous tissue may be done
Duration: Typically 1–3 hours depending on procedure complexity and reconstruction
3) What happens after Mastectomy?
- Recovery monitoring: Observation for bleeding, infection, and pain control
- Pain management: Analgesics and sometimes regional anesthesia
- Activity: Gradual mobilization; avoid heavy lifting until cleared
- Follow-up care: Monitor incision, drains, and wound healing; physical therapy may be recommended
Highlights for post-procedure care:
- ⚡ Swelling, bruising, and mild discomfort are normal
- ⚡ Drain management may be required for 1–2 weeks
- ⚡ Physical therapy or exercises improve shoulder mobility
- ⚡ Psychological support recommended for body image and emotional adjustment
Risks / Benefits
Risks:
- Infection or delayed wound healing
- Bleeding or seroma formation
- Numbness or altered sensation in chest area
- Lymphedema if lymph nodes removed
- Rare complications like flap or implant issues (if reconstructed)
Benefits:
- Removes cancerous tissue and prevents recurrence
- May improve survival in selected patients
- Allows reconstruction for cosmetic and psychological benefits
- Provides peace of mind for high-risk patients
Recovery and Outlook
- Hospital stay: 1–3 days depending on procedure and reconstruction
- Full recovery: 4–6 weeks for basic activities; 2–3 months for full functional recovery
- Long-term outlook: Excellent with appropriate follow-up and adjuvant therapy
- Follow-up: Regular oncologist visits, imaging, and physical therapy if needed
Tips for optimal recovery:
- ✅ Follow drain care and wound instructions
- ✅ Gradually resume daily activities; avoid heavy lifting until cleared
- ✅ Attend follow-up visits for early detection of complications
- ✅ Consider counseling for emotional and psychological support
When To Call the Doctor
- Fever, chills, or signs of infection
- Excessive bleeding or fluid from drains
- Severe pain not relieved by medication
- Redness, swelling, or discharge at incision site
- Signs of lymphedema or limited arm movement
Best Korea Option / Process
Korea provides advanced Mastectomy care:
- Top hospitals: Specialized breast cancer centers with expert surgeons
- Advanced surgical options: Total, modified radical, skin-sparing, and nipple-sparing mastectomies
- Reconstruction: Immediate or delayed options using implants or autologous tissue
- Postoperative care: Pain management, drain monitoring, physical therapy, and psychological support
- International patient support: Online consultation, appointment scheduling, and telemedicine follow-up
Step-by-step process in Korea:
- Preoperative consultation, imaging, and evaluation
- Selection of mastectomy type and reconstruction plan
- Surgery performed under general anesthesia
- Postoperative monitoring, pain management, and physical therapy
- Follow-up visits for wound healing, oncologic management, and long-term care