Overview
Withdrawal bleeding is bleeding that occurs after stopping hormonal contraception or hormone therapy, such as combined oral contraceptives, patches, or hormonal intrauterine devices (IUDs). Unlike a natural menstrual period, it is triggered by the sudden drop in hormones, not by ovulation.
➤ Withdrawal bleeding typically occurs every 21–28 days in women using combined hormonal contraception.
➤ It is usually shorter and lighter than natural menstruation.
➤ In Korea, gynecology clinics provide monitoring, counseling, and management for withdrawal bleeding and hormonal health.
Key Facts
► Definition: Bleeding that occurs during the placebo or hormone-free interval in women taking hormonal contraceptives.
► Prevalence: Common in women using combined hormonal contraceptives; less common with progestin-only methods.
► Associated symptoms: Mild cramping, bloating, breast tenderness, mood changes.
► Risk factors: Inconsistent pill use, hormonal fluctuations, stress, or certain medications.
► Treatment in Korea: Usually not required; counseling and evaluation are provided if bleeding is irregular or prolonged.
What Is Withdrawal Bleeding?
Withdrawal bleeding is a hormone-induced, predictable bleeding event resulting from temporary hormone withdrawal.
➔ Occurs primarily in women using combined oral contraceptives or other hormonal methods.
➔ Usually lasts 3–7 days and is lighter than a natural period.
➔ Unlike menstruation, ovulation does not occur during this time.
➔ May be accompanied by mild premenstrual-like symptoms such as cramping or mood changes.
What Symptoms Are Related to Withdrawal Bleeding?
Symptoms often mimic a natural menstrual period but are generally milder:
→ Light to moderate vaginal bleeding.
→ Mild lower abdominal cramping or discomfort.
→ Breast tenderness or swelling.
→ Mood changes or irritability.
→ Bloating or mild water retention.
→ Headaches or fatigue in some women.
Causes / Possible Causes of Withdrawal Bleeding
Hormonal Causes
➤ Estrogen and progesterone withdrawal – Sudden drop triggers endometrial shedding.
➤ Combined oral contraceptives (COCs) – Placebo week induces predictable bleeding.
➤ Hormone-releasing patches or rings – Withdrawal bleeding occurs during hormone-free interval.
Other Contributing Factors
➔ Missed pills or inconsistent use – May lead to irregular bleeding or spotting.
➔ Stress, illness, or travel – Can disrupt the hormonal rhythm and alter bleeding patterns.
➔ Medications – Certain antibiotics or anticonvulsants may interfere with contraceptive effectiveness.
Underlying Medical Conditions
→ Polycystic ovary syndrome (PCOS) – May cause irregular withdrawal bleeding.
→ Thyroid disorders – Can affect hormonal balance and menstrual patterns.
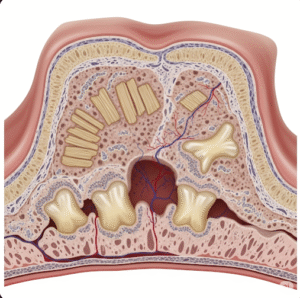
→ Endometrial or uterine abnormalities – Rarely, structural issues may cause abnormal bleeding.
When Should I See My Doctor?
Consult a healthcare provider if:
➤ Bleeding is heavier, prolonged, or unusually painful.
➤ Bleeding occurs outside the expected hormone-free interval.
➤ There are signs of anemia (fatigue, pallor, dizziness).
➤ Bleeding is accompanied by abnormal discharge, odor, or pelvic pain.
➤ Early evaluation ensures proper management of hormonal contraception and detection of underlying conditions.
Care and Treatment
Lifestyle and Self-Care Measures
► Track bleeding patterns and symptoms to distinguish withdrawal bleeding from abnormal bleeding.
► Maintain hydration and a balanced diet to reduce bloating and cramping.
► Use pain relief medications (e.g., acetaminophen or ibuprofen) for mild cramping.
► Practice stress management as emotional stress can influence bleeding patterns.
Medical Treatments
➔ Usually, no treatment is needed for normal withdrawal bleeding.
➔ Adjusting contraceptive regimen – Switching pills, patches, or rings if bleeding is irregular.
➔ Evaluate for underlying endocrine disorders if bleeding is abnormal or prolonged.
➔ Iron supplementation if frequent or heavy bleeding leads to low hemoglobin levels.
Procedural and Advanced Interventions
→ Ultrasound or imaging to assess uterine structure if abnormal bleeding persists.
→ Blood tests – Evaluate thyroid, hormones, or anemia.
→ Endometrial biopsy in rare cases to rule out pathology in persistent or unusual bleeding.
Treatment Options in Korea
Diagnosis in Korea
➤ Gynecological consultation for menstrual pattern assessment.
➤ Laboratory tests to check hormone levels, thyroid function, and anemia.
➤ Imaging studies such as ultrasound to evaluate the uterus and ovaries.
➤ Evaluation for bleeding disorders or systemic conditions if needed.
Non-Surgical Care
► Counseling on proper contraceptive use.
► Adjustment of hormonal contraceptive regimen to reduce irregular bleeding.
► Education on self-monitoring and symptom tracking.
Advanced Care
➔ Management of endocrine disorders or uterine abnormalities contributing to abnormal bleeding.
➔ Multidisciplinary approach with gynecologists and endocrinologists for complex cases.
➔ Follow-up for persistent abnormal bleeding or anemia.
Rehabilitation and Lifestyle Support
→ Guidance on stress management, nutrition, and exercise to support hormonal balance.
→ Patient education for future contraceptive planning and menstrual health awareness.
→ Monitoring for side effects or complications from long-term hormonal therapy.
Korean clinics provide expert gynecological care, personalized contraceptive management, and patient education, ensuring safe and predictable management of withdrawal bleeding.