➤ Overview
A scintillating scotoma is a visual phenomenon in which a person experiences a shimmering, flickering blind spot in their visual field. This often occurs as a type of migraine aura before or during a migraine headache, but it can also appear in other neurological or ophthalmologic conditions. The shimmering spot may expand, move across the visual field, and is sometimes described as zig-zag lines, flashing lights, or geometric patterns.
In Korea, scintillating scotoma is commonly evaluated by neurologists and ophthalmologists, particularly when accompanied by severe headaches or other neurological symptoms. Early consultation can help rule out more serious causes like retinal disease or transient ischemic attacks (TIAs).
➤ Key Facts
→ A scintillating scotoma is typically a migraine-related visual aura.
→ It manifests as shimmering, zig-zag, or flickering blind spots in the vision.
→ The condition may last from 5 minutes up to an hour.
→ Often occurs before a migraine headache, but can appear independently.
→ Usually benign, but persistent or unusual patterns require evaluation.
→ Can be associated with neurological conditions in rare cases.
→ In Korea, diagnosis includes eye exams, neurological assessments, and imaging if needed.
➤ What is Scintillating Scotoma?
A scintillating scotoma is a temporary visual disturbance in the central or peripheral visual field. It typically starts as a small blind spot, surrounded by flickering or flashing lights, and gradually expands. Patients often describe seeing zig-zag patterns, sparkles, or “C-shaped” lights that slowly move across their vision.
It is most commonly linked to migraine with aura, but can also occur due to ocular migraines, retinal migraine, or other neurological disorders. In Korean medical practice, careful differentiation between benign migraine aura and serious retinal or neurological disease is essential.
➤ What Symptoms are Related to Scintillating Scotoma?
Symptoms accompanying scintillating scotoma may include:
→ Temporary visual loss or blind spots in the affected area.
→ Flickering lights, sparkles, or zig-zag patterns.
→ Headache or migraine, often following the visual disturbance.
→ Nausea or vomiting, sometimes associated with migraine.
→ Sensitivity to light (photophobia) or sound (phonophobia).
→ Rarely, numbness, tingling, or speech difficulties if linked to complex migraine aura.
→ Fatigue or dizziness after the episode ends.
➤ What Causes / Possible Causes?
Scintillating scotoma arises from temporary changes in the brain or eye’s visual processing. Common causes include:
→ Migraine with aura – The most frequent cause, due to cortical spreading depression in the visual cortex.
→ Ocular migraine – Changes in retinal blood flow cause temporary visual disturbances.
→ Retinal disease – Rarely, retinal detachment or vascular occlusion.
→ Transient ischemic attacks (TIA) – Sudden, temporary interruption of blood flow to the brain.
→ Medication side effects – Certain drugs can trigger visual auras.
→ Stress, fatigue, or hormonal changes – Can precipitate migraine auras.
→ Genetic predisposition – Migraine with aura often runs in families.
➤ When Should I See My Doctor?
Although scintillating scotoma is usually benign, medical evaluation is essential if any of the following occur:
→ First-time occurrence, especially in adults over 40.
→ Sudden, severe, or prolonged visual changes.
→ Accompanied by weakness, speech difficulties, or facial drooping.
→ Visual disturbances lasting longer than one hour.
→ Headache-free scotomas appearing frequently or worsening.
→ If you have underlying vascular risk factors like hypertension, diabetes, or high cholesterol.
➤ Care and Treatment
Treatment focuses on managing underlying causes, mainly migraines, and reducing triggers:
→ Identify and avoid migraine triggers – such as certain foods, stress, or sleep disruption.
→ Medications – Acute treatments may include triptans or NSAIDs; preventive therapies may be prescribed for frequent migraines.
→ Hydration and rest – Proper fluid intake and regular sleep patterns help prevent episodes.
→ Eye protection – Sunglasses and minimizing screen glare can reduce visual strain.
→ Lifestyle modifications – Stress management, regular exercise, and balanced diet.
→ Monitoring – Keep a migraine diary to track aura patterns and triggers.
➤ Treatment Options in Korea
South Korea provides advanced migraine and neurological care, including:
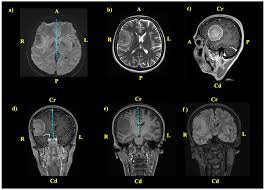
Diagnosis in Korea
→ Comprehensive eye examination to rule out retinal causes.
→ Neurological assessment for cortical or vascular issues.
→ Imaging studies like MRI or CT scans if atypical features are present.
Medical Treatments in Korea
→ Migraine-specific medications (triptans, beta-blockers, or anticonvulsants).
→ Preventive therapies for chronic migraine sufferers.
→ Supplements – Magnesium, riboflavin (Vitamin B2), or Coenzyme Q10 may be recommended.
Advanced Therapies in Korea
→ Neuromodulation devices for patients with refractory migraines.
→ Botulinum toxin injections for chronic migraine management.
→ Integrated approaches combining Western medicine with traditional Korean therapies (e.g., acupuncture or herbal remedies) to reduce aura frequency.
Rehabilitation & Support in Korea
→ Patient education on migraine triggers and aura management.
→ Lifestyle counseling for stress reduction, sleep hygiene, and diet modification.
→ Ongoing monitoring by neurologists and ophthalmologists to prevent complications.