Overview
Myoclonus refers to sudden, involuntary muscle jerks or twitches that can occur in a single muscle or a group of muscles. These twitches can be brief, repetitive, or rhythmic, and while often harmless, they may sometimes signal an underlying neurological or systemic condition. Myoclonus can affect any part of the body, including the arms, legs, face, and trunk.
In Korea, myoclonus is evaluated and treated in neurology and specialized movement disorder clinics, where physicians differentiate between benign and pathological causes using advanced diagnostic tools and tailored therapies.
Key Facts
➤ Myoclonus consists of sudden, involuntary muscle jerks.
➤ It may occur sporadically, in clusters, or rhythmically.
➤ Causes range from benign stress-related twitches to neurological disorders.
➤ Myoclonus can be classified by timing, trigger, and underlying pathology.
➤ In Korea, treatment involves neurological assessment, medications, and supportive care to reduce symptoms and improve quality of life.
What is Myoclonus?
Myoclonus is a rapid, involuntary contraction of one or more muscles. The movement is typically:
➔ Sudden and brief – lasting milliseconds to a few seconds.
➔ Shock-like or jerky – may resemble a startle or twitch.
➔ Localized or generalized – affecting a single limb or multiple muscle groups.
Types of myoclonus include:
- Physiological myoclonus – occurs normally, such as hiccups or sleep-related twitches.
- Essential myoclonus – occurs without underlying disease; often benign and hereditary.
- Epileptic myoclonus – associated with seizure disorders.
- Secondary myoclonus – due to neurological diseases, metabolic disorders, or drug reactions.
Symptoms Related to Myoclonus
➤ Sudden, involuntary jerks or twitches of muscles.
➤ Twitches that can be occasional or frequent.
➤ Muscle movements may interfere with daily activities or sleep.
➤ Sometimes accompanied by weakness, numbness, or tremors depending on underlying cause.
➤ Visual disturbance or coordination difficulties if myoclonus is part of a neurological disorder.
Causes / Possible Causes
Myoclonus can be triggered by a variety of neurological, metabolic, and physiological factors:
Physiological Causes
➤ Sleep-related jerks (hypnic jerks) – occur when falling asleep.
➤ Stress, fatigue, or anxiety-induced muscle twitches.
➤ Sudden startle responses or reflex jerks.
Neurological Causes
➤ Epilepsy, especially juvenile myoclonic epilepsy.
➤ Neurodegenerative disorders such as Parkinson’s disease, Alzheimer’s, or Huntington’s disease.
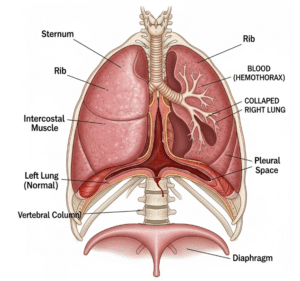
➤ Brain or spinal cord injury.
➤ Stroke or brain lesions affecting motor pathways.
Metabolic and Systemic Causes
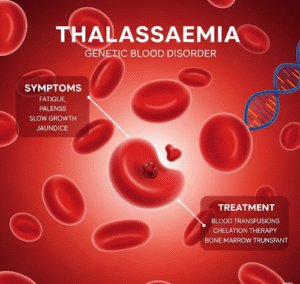
➤ Electrolyte imbalances, including low calcium, magnesium, or potassium.
➤ Kidney or liver failure causing toxic metabolic myoclonus.
➤ Adverse reactions to certain medications (e.g., antidepressants, anticonvulsants).
Other Contributing Factors
➤ Infections affecting the nervous system.
➤ Autoimmune disorders impacting motor neurons.
➤ Vitamin deficiencies (B12, folate) affecting neuromuscular function.
Risk Factors
➤ Family history of neurological disorders or essential myoclonus.
➤ Age – certain types of myoclonus are more common in older adults.
➤ Underlying neurological or metabolic disease.
➤ Use of medications known to trigger myoclonus.
➤ Sleep deprivation, fatigue, or high stress levels.
Complications
While benign myoclonus is generally harmless, pathological myoclonus may cause:
➤ Interference with daily activities such as writing, eating, or walking.
➤ Sleep disturbances leading to fatigue or cognitive impairment.
➤ Emotional distress due to visible involuntary movements.
➤ Increased risk of falls or injury in severe cases.
➤ Underlying neurological disease progression if secondary causes are untreated.
When Should I See My Doctor?
Seek medical attention if:
➤ Muscle jerks are frequent, persistent, or worsening.
➤ Myoclonus is associated with seizures, weakness, numbness, or coordination issues.
➤ Twitches interfere with daily activities or sleep.
➤ Occur alongside confusion, vision changes, or cognitive impairment.
➤ You have risk factors such as neurological disease, metabolic disorders, or medication use.
Early evaluation ensures proper diagnosis, treatment, and management of potential underlying causes.
Care and Treatment
Lifestyle and Home Measures
➤ Reduce stress, practice relaxation techniques, and maintain proper sleep hygiene.
➤ Gentle stretching or physical therapy exercises to relax muscles.
➤ Avoid stimulants like caffeine that may worsen twitching.
➤ Maintain hydration and balanced nutrition to support neuromuscular health.
Medical Treatments
➤ Medications – anticonvulsants (e.g., clonazepam, valproate) for epileptic myoclonus.
➤ Treat underlying conditions – metabolic, infectious, or neurological disorders.
➤ Botulinum toxin injections for severe localized myoclonus.
➤ Physical or occupational therapy to improve functional ability.
Preventive Measures
➤ Proper stress management and sleep routines.
➤ Avoid triggering medications when possible.
➤ Manage underlying neurological or metabolic conditions.
➤ Regular medical checkups for early detection of systemic causes.
Treatment Options in Korea
Korea offers advanced neurological care for patients with myoclonus:
Diagnostic Services
➤ Electroencephalogram (EEG) for seizure-related myoclonus.
➤ MRI or CT scans for structural brain or spinal cord evaluation.
➤ Blood tests for electrolyte imbalances, liver and kidney function.
➤ Comprehensive neurological assessments by movement disorder specialists.
Therapies and Supportive Care
➤ Prescription anticonvulsants and muscle relaxants tailored to the type of myoclonus.
➤ Physical therapy and occupational therapy for motor function improvement.
➤ Integrative treatments such as acupuncture or traditional Korean medicine for symptomatic relief.
➤ Multidisciplinary care combining neurology, rehabilitation, and pain management.
✅ In summary: Myoclonus is a sudden, involuntary muscle twitch that can be benign or indicate underlying neurological or metabolic conditions. While often harmless, persistent or severe cases require evaluation. In Korea, patients benefit from advanced diagnostics, tailored medications, rehabilitation, and integrative therapies to control symptoms, improve function, and address underlying causes.