Overview
Incontinence after prostate surgery is a common complication affecting men who have undergone procedures such as radical prostatectomy, transurethral resection of the prostate (TURP), or minimally invasive prostate surgeries. It refers to the involuntary leakage of urine, ranging from mild dribbling to complete loss of bladder control.
In South Korea, urology specialists and rehabilitation centers provide comprehensive management for post-prostate surgery incontinence, including diagnostic assessment, pelvic floor therapy, medications, and surgical interventions for persistent cases.
Key Facts
🟢 ➤ Urinary incontinence can occur in up to 20–40% of men immediately after prostate surgery.
🟢 ➤ The severity usually decreases over time, with most men regaining significant bladder control within 6–12 months.
🟢 ➤ Risk factors include age, pre-existing bladder problems, type of surgery, and nerve-sparing techniques.
🟢 ➤ Types of post-surgical incontinence include stress incontinence, urge incontinence, and mixed incontinence.
🟢 ➤ Diagnosis involves clinical evaluation, urinalysis, bladder scans, urodynamic testing, and sometimes imaging.
🟢 ➤ Management includes lifestyle modifications, pelvic floor exercises, medications, and surgical options in severe or persistent cases.
What is Incontinence After Prostate Surgery?
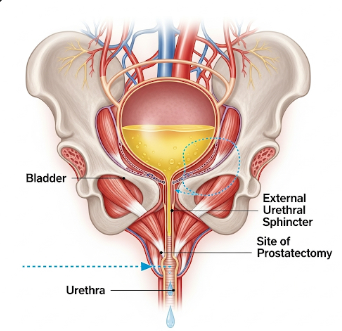
Post-prostate surgery incontinence occurs when the urinary sphincter or bladder control mechanisms are weakened or disrupted during surgery.
➤ Stress incontinence: leakage during activities that increase abdominal pressure, such as coughing, sneezing, or lifting.
➤ Urge incontinence: sudden, strong urges to urinate with involuntary leakage.
➤ Mixed incontinence: a combination of stress and urge symptoms.
➤ Severity varies from minor dribbling to complete loss of control, affecting quality of life, social interactions, and mental health.
Symptoms Related to Incontinence After Prostate Surgery
Symptoms depend on the type and severity of incontinence:
🟢 ➤ Dribbling urine or inability to hold urine after sneezing, coughing, or physical exertion.
🟢 ➤ Sudden, strong urges to urinate followed by leakage.
🟢 ➤ Frequent trips to the bathroom or waking at night to urinate (nocturia).
🟢 ➤ Skin irritation or infections due to constant wetness.
🟢 ➤ Emotional distress, embarrassment, and reduced participation in social activities.
Causes / Possible Causes
Urinary incontinence after prostate surgery occurs due to damage, weakening, or disruption of urinary control structures:
Sphincter Weakness
➤ Surgery may impair the external urinary sphincter, reducing the ability to hold urine under stress.
Bladder Dysfunction
➤ Temporary changes in bladder capacity or overactivity can lead to urge incontinence.
Nerve Damage
➤ Injury to nerves controlling bladder and sphincter function may occur during surgery, particularly if nerve-sparing techniques are not used.
Pre-existing Conditions
➤ Older age, previous urinary issues, or comorbidities like diabetes may increase risk.
Type of Surgery
➤ Radical prostatectomy carries higher risk compared to minimally invasive procedures, although robotic-assisted surgery can reduce complications.
When Should I See a Doctor?
Seek medical advice if:
🟢 ➤ Incontinence persists beyond a few weeks after surgery.
🟢 ➤ There is severe leakage affecting daily life, work, or sleep.
🟢 ➤ Recurrent urinary tract infections or skin irritation occur.
🟢 ➤ Sudden changes in urinary patterns or severe pain develop.
🟢 ➤ There is concern about surgical complications such as strictures or residual cancer-related issues.
Early consultation ensures targeted management, improved recovery, and prevention of secondary complications.
Care and Treatment
Management of post-prostate surgery incontinence focuses on gradual improvement, symptom control, and quality of life enhancement:
Lifestyle and Home Measures
➤ Limit caffeine and alcohol, which can irritate the bladder.
➤ Maintain healthy weight to reduce abdominal pressure on the bladder.
➤ Schedule regular bathroom visits and avoid delaying urination.
Pelvic Floor Exercises (Kegel Exercises)
➤ Strengthen pelvic muscles to improve sphincter control.
➤ Perform daily under guidance from a physiotherapist or urologist.
➤ Biofeedback therapy may help men identify and strengthen the correct muscles.
Medications
➤ Anticholinergics for bladder overactivity.
➤ Alpha-blockers for urinary flow improvement in select cases.
Surgical and Advanced Treatments
➤ Male sling procedures: reposition and support the urethra for stress incontinence.
➤ Artificial urinary sphincters: implantable devices that provide controllable bladder closure.
➤ Bulking agents: injectable materials to improve urethral closure in mild cases.
Advanced Care in Korea
➤ South Korean urology centers provide state-of-the-art robotic-assisted prostate surgery, pelvic floor rehabilitation, and surgical management for persistent incontinence.
➤ Multidisciplinary care includes urologists, physiotherapists, and nursing specialists for personalized recovery plans.
➤ Patients receive education on bladder training, symptom monitoring, and strategies for social confidence.
Highlights (Clean Green Arrow Version)
🟢 ➤ Post-prostate surgery incontinence is involuntary urine leakage due to sphincter or bladder control disruption.
🟢 ➤ Symptoms: dribbling, urgency, frequent urination, nocturia, skin irritation, and emotional distress.
🟢 ➤ Causes: sphincter weakness, bladder dysfunction, nerve damage, pre-existing conditions, or type of surgery.
🟢 ➤ Seek medical care for persistent leakage, severe symptoms, infections, or sudden urinary changes.
🟢 ➤ Treatments include lifestyle modifications, pelvic floor exercises, medications, and surgical interventions.
🟢 ➤ South Korea offers advanced urology care with robotic-assisted surgery, multidisciplinary rehabilitation, and personalized management for optimal recovery.