Overview
Foamy urine refers to urine that appears bubbly or frothy, often resembling soap suds. While occasional foamy urine is generally harmless, persistent or excessive foaming may indicate underlying kidney problems or systemic conditions. It occurs due to rapid urination, high protein content, or kidney dysfunction affecting the filtration system. In Korea, nephrology and urology clinics provide comprehensive evaluation of foamy urine, including urinalysis, blood tests, imaging, and kidney function assessment, followed by targeted treatment to address the underlying causes.
Highlights:
➤ Persistent foamy urine may indicate kidney or urinary tract issues
➤ Intermittent foaming is often benign and related to urination habits
➤ Early evaluation helps prevent progression of kidney disease
Key Facts
➤ Prevalence: Common; intermittent foamy urine occurs in healthy individuals, while persistent foamy urine is less common and clinically significant
➤ Age affected: Can occur at any age, more concerning in adults with risk factors for kidney disease
➤ Gender: Affects both males and females
➤ Impact: May signal proteinuria, kidney damage, or systemic conditions
➤ Prognosis: Depends on underlying cause; early detection of kidney problems can improve outcomes
What is Foamy Urine?
Foamy urine occurs when gas bubbles form in the urine, often due to rapid urination or protein content. The foam is typically temporary and harmless if it disappears with slower urination. Persistent foam may suggest proteinuria, which is an indicator of glomerular or kidney damage. Key mechanisms include:
- Mechanical: Urine hitting the toilet rapidly can trap air, creating bubbles
- Chemical: Presence of detergents or urine supplements
- Pathological: High protein levels in urine, kidney disease, or infections
Highlights:
➤ Foamy urine can be benign or a sign of serious kidney disease
➤ Persistent or worsening foam warrants medical assessment
➤ Color, odor, and associated symptoms provide diagnostic clues
What Symptoms Are Related to Foamy Urine?
➤ Bubbly or frothy urine – May appear white, yellow, or slightly cloudy
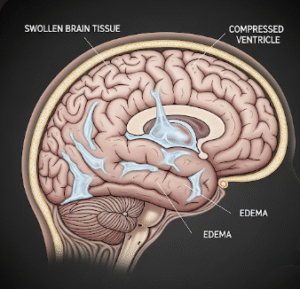
➤ Swelling (edema): Often in the face, hands, feet, or abdomen if protein loss is significant
➤ Changes in urine volume or frequency – Polyuria or oliguria
➤ Urinary discomfort or pain: Indicates infection or inflammation
➤ Fatigue or weakness: May reflect kidney dysfunction or protein loss
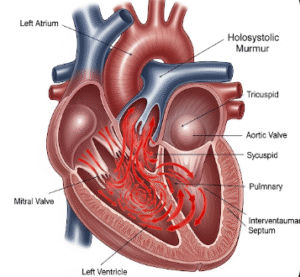
➤ Associated systemic symptoms: High blood pressure, nausea, or foamy urine in chronic kidney disease
Highlights:
➣ Foamy urine is a visible sign that can help detect kidney issues early
➣ Combination with edema or hypertension is clinically significant
What Causes / Possible Causes
➤ Rapid urination: Temporary foam due to velocity of urine flow
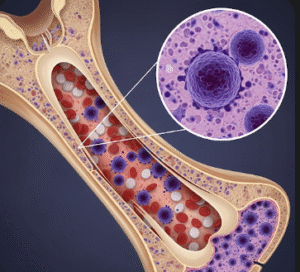
➤ Proteinuria: Excess protein in urine caused by kidney diseases such as:
- Glomerulonephritis
- Diabetic nephropathy
- Hypertension-related kidney damage
➤ Urinary tract infections: Can sometimes produce foamy or cloudy urine
➤ Kidney damage or disease: Acute or chronic renal dysfunction
➤ Dehydration: Concentrated urine may foam
➤ Chemical exposure: Detergents in toilet or urine collection containers
➤ Rare causes: Nephrotic syndrome, preeclampsia in pregnancy
Highlights:
➣ Persistent foam is often associated with proteinuria and kidney disease
➣ Identifying the underlying cause is crucial for management
When Should I See My Doctor?
➤ Persistent or increasing foamy urine
➤ Accompanied by swelling, fatigue, or high blood pressure
➤ Presence of pain, burning, or blood in urine
➤ Underlying diabetes, hypertension, or kidney disease
➤ Sudden change in urine color, odor, or frequency
Highlights:
➣ Consultation at a Korean nephrology or urology clinic is recommended for persistent foam
➣ Early evaluation can prevent progression of kidney damage
Care and Treatment
➤ Initial assessment: Urinalysis to detect protein, blood, or infection
➤ Blood tests: Kidney function tests including creatinine, BUN, and eGFR
➤ Imaging: Ultrasound or CT scan to evaluate kidney structure
➤ Lifestyle modifications: Adequate hydration, balanced diet, and control of blood pressure
➤ Medications:
- ACE inhibitors or ARBs to reduce proteinuria
- Antibiotics for urinary tract infections
- Diuretics for edema if present
➤ Monitoring: Regular follow-up with urine and blood tests
➤ Advanced interventions: Kidney biopsy in cases of unexplained persistent proteinuria
Highlights:
➣ Treatment is cause-specific, focusing on kidney health and systemic management
➣ Lifestyle changes plus medical therapy can significantly improve outcomes
Treatment Options in Korea
Medical Treatments:
➤ Nephrology clinics: Comprehensive kidney assessment, urinalysis, and blood tests
➤ Urology clinics: Evaluation of urinary tract and related conditions
➤ Dietitian services: Personalized nutrition plans to support kidney function
Advanced Procedures:
➤ Kidney biopsy: For unexplained or severe proteinuria
➤ Dialysis: In cases of chronic kidney failure
➤ Hospitalization: For acute kidney injury or nephrotic syndrome
➤ Follow-up care: Continuous monitoring of kidney function, proteinuria, and blood pressure
Rehabilitation & Follow-Up Care:
➤ Education on hydration, diet, and early detection of complications
➤ Regular urine and blood tests to track kidney health
➤ Multidisciplinary support for long-term renal care and lifestyle adjustments
Highlights:
➣ Korean clinics provide advanced diagnostics, individualized therapy, and long-term monitoring
➣ Early and appropriate intervention improves kidney outcomes and quality of life