Overview
Autoantibodies are antibodies produced by the immune system that mistakenly target and react with a person’s own tissues or organs. They are a hallmark of autoimmune diseases and play a critical role in diagnosing and monitoring these conditions. While the presence of autoantibodies does not always indicate disease, their detection can reveal immune system dysregulation or risk for developing autoimmune disorders.
In South Korea, specialized laboratories, immunology clinics, and autoimmune disease centers provide comprehensive testing, diagnosis, and management for patients with suspected autoantibody-related conditions. Early detection allows for timely treatment and better long-term outcomes.
Key Facts
Highlights:
➡️ Autoantibodies are immune proteins that mistakenly attack the body’s own cells and tissues.
➡️ They are associated with autoimmune diseases such as lupus, rheumatoid arthritis, and Hashimoto’s thyroiditis.
➡️ Detection of autoantibodies helps in diagnosis, disease monitoring, and treatment planning.
➡️ Not all autoantibodies cause disease; some may be present in healthy individuals without symptoms.
➡️ South Korea offers advanced immunology labs for precise autoantibody testing and clinical interpretation.
What is Autoantibodies?
Autoantibodies are antibodies directed against the body’s own proteins, cells, or tissues. Under normal circumstances, the immune system produces antibodies to fight infections or foreign substances. In autoimmune conditions, the immune system loses tolerance to self-antigens, resulting in autoantibody production.
Common types include:
- Antinuclear Antibodies (ANA): Often associated with systemic lupus erythematosus.
- Rheumatoid Factor (RF): Seen in rheumatoid arthritis.
- Anti-Thyroid Antibodies: Such as anti-thyroid peroxidase (TPO) in Hashimoto’s thyroiditis.
- Anti-DsDNA Antibodies: Specific for lupus.
- Anti-CCP (Cyclic Citrullinated Peptide): Highly specific for rheumatoid arthritis.
These antibodies can cause tissue damage directly, trigger inflammation, or serve as biomarkers to guide diagnosis and treatment.
What Symptoms are Related to Autoantibodies?
Symptoms vary depending on the specific autoimmune condition associated with the autoantibodies:
- Joint Pain and Swelling: Common in rheumatoid arthritis.
- Fatigue and Fever: Seen in systemic autoimmune disorders.
- Skin Rashes: Such as the butterfly rash in lupus.
- Thyroid Dysfunction: Hypothyroidism or hyperthyroidism in thyroid autoimmunity.
- Organ-Specific Symptoms: Kidney involvement, lung inflammation, or gastrointestinal issues.
- Neurological Symptoms: Numbness, weakness, or cognitive changes in certain autoimmune neuropathies.
The presence of autoantibodies often correlates with disease activity, guiding treatment decisions.
What Causes / Possible Causes of Autoantibodies?
Highlights:
➡️ Genetic Predisposition: Certain genes increase susceptibility to autoimmune disorders.
➡️ Environmental Triggers: Viral infections, toxins, or certain medications can provoke autoantibody production.
➡️ Hormonal Factors: Women are more likely to develop autoimmune diseases, possibly due to estrogen effects.
➡️ Immune Dysregulation: Failure of immune tolerance mechanisms allows self-reactive B cells to produce autoantibodies.
➡️ Chronic Inflammation: Persistent immune activation can trigger autoantibody generation.
➡️ Epigenetic Changes: Modifications in gene expression may contribute to autoimmune responses.
When Should I See My Doctor?
Highlights:
➡️ If you experience unexplained fatigue, joint pain, swelling, or skin rashes.
➡️ If you have symptoms suggestive of thyroid dysfunction (weight changes, palpitations, or hair loss).
➡️ For recurrent or unusual symptoms affecting multiple organs that could indicate systemic autoimmune disease.
➡️ If you have a family history of autoimmune disorders, early testing may help identify risk.
➡️ Early assessment improves outcomes, allowing for targeted treatment before significant organ damage occurs.
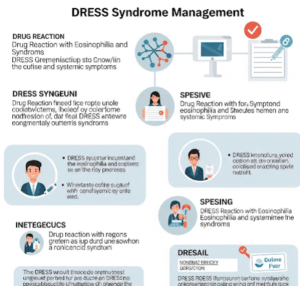
Care and Treatment
Management focuses on treating the underlying autoimmune disease and modulating the immune system to reduce autoantibody effects:
Highlights:
➡️ Immunosuppressive Medications: Corticosteroids, methotrexate, or biologics to control inflammation.
➡️ Symptomatic Treatment: Pain management, physical therapy, and supportive care for organ-specific symptoms.
➡️ Monitoring Autoantibody Levels: Regular lab tests to assess disease activity and treatment response.
➡️ Lifestyle Modifications: Balanced diet, exercise, and stress reduction to support immune health.
➡️ Patient Education: Understanding triggers, medication adherence, and early recognition of flares.
➡️ Specialist Care: Rheumatologists, endocrinologists, nephrologists, or neurologists depending on organ involvement.
➡️ Emerging Therapies: Novel biologics or targeted immunotherapies are increasingly available in specialized centers.
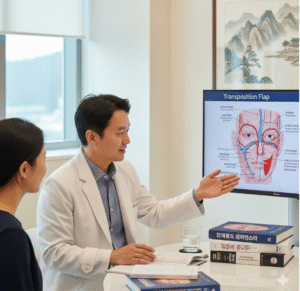
Treatment Options in Korea
South Korea provides comprehensive evaluation and management for patients with autoantibody-related conditions:
Highlights:
➡️ Advanced Immunology Laboratories: Testing for ANA, RF, anti-CCP, thyroid antibodies, and other markers.
➡️ Specialized Rheumatology and Endocrinology Clinics: Personalized treatment plans for autoimmune disorders.
➡️ Biologic Therapy Centers: Administration of advanced immunomodulatory medications.
➡️ Multidisciplinary Care: Collaboration between rheumatologists, endocrinologists, nephrologists, and neurologists.
➡️ Monitoring and Follow-Up: Long-term tracking of autoantibody levels and organ function.
➡️ Rehabilitation Services: Physical and occupational therapy for musculoskeletal involvement.
➡️ Medical Tourism Support: Multilingual services, structured diagnostic pathways, and follow-up care for international patients.