Overview
Buruli Ulcer (BU) is a rare but serious skin infection caused by the bacterium Mycobacterium ulcerans. It typically begins as a small painless nodule or papule on the skin, which gradually enlarges and develops into a large ulcer with undermined edges. The infection can affect skin, soft tissue, and occasionally bone, leading to disfigurement, functional impairment, and long-term complications if untreated.
Although Buruli Ulcer is most common in West and Central Africa, cases occasionally occur in travelers or immigrants in Korea. Korean healthcare provides advanced diagnostic tools, medical management, and reconstructive surgery for patients affected by BU.
What is Buruli Ulcer?
Buruli Ulcer is a chronic, necrotizing skin infection caused by M. ulcerans, a slow-growing mycobacterium. The disease is characterized by:
- Initial painless skin lesion, often misdiagnosed as an insect bite or minor injury
- Progressive ulceration, with a necrotic base and undermined edges
- Potential bone involvement in severe or untreated cases
- Slow progression, sometimes over weeks to months, without systemic symptoms initially
The infection is non-contagious and primarily transmitted through environmental exposure, often via contaminated water or soil, though the exact mode of transmission remains unclear.
Symptoms
Symptoms of Buruli Ulcer evolve as the infection progresses:
- Small painless nodule or papule at the site of infection
- Swelling or localized edema around the lesion
- Progressive ulcer formation, often with a necrotic center and raised edges
- Pain or discomfort may develop as the ulcer enlarges or becomes secondarily infected
- Bone involvement, causing swelling, deformity, or limited movement in advanced cases
- Functional impairment, particularly if the lesion affects joints or extremities
- Secondary infection, leading to redness, pus, or foul odor
Early recognition of these symptoms is critical for effective treatment and prevention of severe complications.
Causes
Buruli Ulcer is caused by infection with Mycobacterium ulcerans:
- The bacterium produces mycolactone, a toxin that destroys skin and subcutaneous tissue
- Infection usually occurs through minor trauma or abrasions in contaminated environments
- Transmission is often associated with swampy areas, slow-moving water, or insect vectors, though definitive vectors are still under investigation
- Risk is increased with prolonged exposure to contaminated water or soil
Unlike other mycobacterial infections, Buruli Ulcer is not typically transmitted person-to-person.
Risk Factors
- Living in or visiting endemic areas, including swampy or rural regions
- Repeated exposure to contaminated water or soil
- Skin injuries, such as cuts, insect bites, or abrasions
- Immunocompromised individuals, including those with HIV/AIDS
- Young children, who are more frequently affected in endemic regions
Complications
If untreated, Buruli Ulcer can lead to serious local and systemic complications:
- Extensive skin and soft tissue necrosis
- Secondary bacterial infection causing additional pain and delayed healing
- Scarring and disfigurement, which may be permanent
- Functional impairment, particularly if lesions involve joints, tendons, or bones
- Chronic ulcers that are difficult to treat
- Psychological distress due to appearance changes and long-term disability
Prevention
While Buruli Ulcer cannot be completely prevented, several strategies may reduce risk of infection:
- Avoiding prolonged contact with stagnant or contaminated water
- Protective clothing such as long sleeves and trousers when in endemic areas
- Prompt cleansing and care of skin injuries to prevent bacterial entry
- Early medical evaluation for suspicious skin lesions
- Awareness campaigns in at-risk communities to educate about risk and early symptoms
Treatment Options in Korea
Diagnosis
Diagnosis involves clinical evaluation, laboratory testing, and imaging:
- Physical examination of skin lesions, noting size, shape, and progression
- Laboratory confirmation, including PCR testing for M. ulcerans DNA
- Histopathology to detect characteristic necrosis and inflammatory changes
- Culture of the bacterium, though it grows slowly and is rarely used for rapid diagnosis
- Imaging studies (X-ray, MRI) if bone involvement is suspected
Medical Management
Medical treatment focuses on antimicrobial therapy and infection control:
- Combination antibiotic therapy, typically rifampicin plus clarithromycin or moxifloxacin, for 8 weeks
- Wound care, including cleaning, debridement, and dressing changes
- Pain management and supportive care to maintain patient comfort
- Monitoring for secondary infections to prevent complications
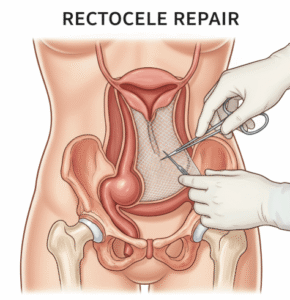
Surgical Interventions
Surgery may be necessary in advanced cases to remove necrotic tissue or restore function:
- Debridement of necrotic skin and subcutaneous tissue
- Skin grafting or flap surgery to close large ulcers
- Orthopedic procedures if bones or joints are affected
- Postoperative rehabilitation, including physical therapy to regain mobility and function
Supportive Care
- Nutritional support to promote healing
- Psychological support, as prolonged ulcers and disfigurement may impact mental health
- Long-term follow-up to monitor healing and prevent recurrence
Prognosis
With timely treatment, the prognosis of Buruli Ulcer is generally favorable:
- Early-stage lesions respond well to antibiotics, with minimal scarring
- Advanced lesions may require surgery but can heal with proper care
- Long-term functional recovery is possible, particularly with rehabilitation and wound management
- Delayed treatment increases the risk of complications, including permanent disfigurement and disability
Buruli Ulcer management in Korea combines rapid diagnosis, effective antibiotic therapy, advanced surgical care, and multidisciplinary rehabilitation, ensuring that patients achieve optimal healing, restored function, and improved quality of life.