Overview
Breast infections refer to infections of the breast tissue, typically caused by bacteria, viruses, or, rarely, fungi. They can occur in lactating and non-lactating women, with lactational infections (mastitis) being the most common. Symptoms can range from pain, swelling, and redness to fever and systemic illness.
In Korea, breast infections are managed in hospitals, breast clinics, and maternity centers using antibiotics, imaging-guided procedures, and supportive care. Korean medical facilities prioritize early diagnosis and minimally invasive treatment to relieve symptoms, prevent abscess formation, and preserve breast health.
What is a Breast Infection?
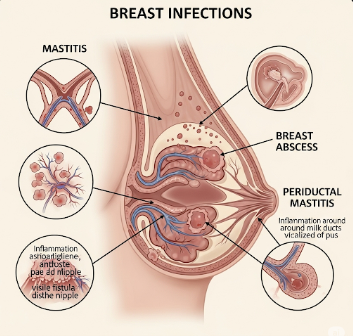
A breast infection occurs when microorganisms invade breast tissue, triggering an inflammatory response. The most common infections include:
- Mastitis: Infection in lactating women, often caused by Staphylococcus aureus
- Non-lactational breast infections: Occur due to duct obstruction, trauma, or underlying conditions
- Breast abscess: A localized collection of pus from untreated infection
- Periductal mastitis: Infection of the ducts near the nipple, often associated with smoking
Breast infections can be acute or chronic, and prompt treatment is essential to prevent complications.
Symptoms
Symptoms vary depending on the type and severity of the infection:
- Breast pain and tenderness
- Swelling or lump in the affected area
- Redness and warmth of the skin
- Fever and malaise in more severe infections
- Nipple discharge, sometimes purulent
- Fatigue and discomfort during breastfeeding in lactating women
- Skin changes, including dimpling or ulceration in chronic infections
Causes
Breast infections are caused by microbial invasion and obstruction of normal drainage:
- Bacterial infections: Most commonly Staphylococcus aureus or Streptococcus species
- Blocked milk ducts during lactation leading to mastitis
- Cracked or sore nipples allowing bacterial entry
- Trauma or injury to the breast tissue
- Underlying chronic conditions such as diabetes or immunodeficiency
- Smoking, which increases the risk of periductal mastitis
Risk Factors
- Lactation: Particularly in the first few weeks postpartum
- Improper breastfeeding techniques
- Previous breast infections or abscesses
- Cracked, sore, or irritated nipples
- Diabetes or immunocompromised states
- Smoking
- Obesity or poor hygiene
Complications
Untreated or severe breast infections can lead to:
- Breast abscess formation requiring drainage
- Chronic infections or recurrent mastitis
- Sepsis if infection spreads to the bloodstream
- Permanent tissue damage or scarring
- Interference with breastfeeding
- Fistula formation in rare chronic cases
Prevention
Preventive measures focus on hygiene, breastfeeding care, and early intervention:
- Proper breastfeeding techniques to prevent blocked ducts and nipple trauma
- Regular breast emptying during lactation
- Maintaining nipple hygiene
- Prompt treatment of mastitis or minor infections
- Avoid smoking
- Healthy diet and lifestyle to support immune function
- Routine breast examinations for early detection of infections
Treatment Options in Korea
Diagnosis
Early diagnosis is crucial for preventing complications:
- Physical examination: Detects tenderness, swelling, and warmth
- Ultrasound imaging: Identifies abscesses or duct obstruction
- Mammography or MRI: Used for atypical or chronic cases
- Microbiological culture: Determines the specific pathogen for targeted antibiotics
- Blood tests: Assess systemic infection
Medical Management
- Antibiotics: Oral or intravenous antibiotics targeting Staphylococcus aureus or other identified bacteria
- Pain management: Analgesics for discomfort
- Supportive care: Warm compresses and adequate hydration
- Breastfeeding support: Ensures continued milk flow and reduces milk stasis
Drainage Procedures
- Needle aspiration: Ultrasound-guided drainage for small to moderate abscesses
- Incision and drainage (I&D): Surgical drainage for large, multiloculated, or resistant abscesses
- Minimally invasive techniques in Korean hospitals reduce scarring and preserve breast tissue
Post-treatment Care
- Follow-up imaging to ensure complete resolution
- Continued antibiotics as prescribed
- Proper breastfeeding guidance for lactating women
- Hygiene measures to prevent recurrence
- Psychological support if infection affects breastfeeding or quality of life
Prognosis
With timely treatment, the prognosis for breast infections is excellent:
- Early antibiotic therapy and drainage typically resolve symptoms quickly
- Minimally invasive procedures minimize tissue damage and scarring
- Complications are rare when treated promptly in Korea’s specialized clinics
- Lactating women can often continue breastfeeding safely
- Long-term follow-up ensures early detection of recurrence and management of underlying risk factors
Korean hospitals and breast clinics provide comprehensive care for breast infections, combining advanced diagnostics, targeted antibiotics, minimally invasive drainage, and patient education, ensuring optimal recovery, prevention of recurrence, and preservation of breast health.