Overview
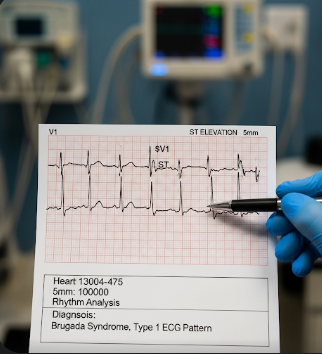
Brugada Syndrome (BrS) is a genetic cardiac disorder characterized by abnormal electrical activity in the heart, leading to an increased risk of sudden cardiac arrest. This condition primarily affects the right ventricle and its conduction pathways, often presenting with distinctive patterns on an electrocardiogram (ECG).
In Korea, Brugada Syndrome is managed in cardiology and electrophysiology centers, where patients receive genetic counseling, advanced diagnostics, and preventive treatment strategies. Korean healthcare emphasizes early detection, lifestyle management, and cutting-edge interventions to reduce the risk of life-threatening arrhythmias.
What is Brugada Syndrome?
Brugada Syndrome is an inherited cardiac channelopathy caused by mutations in the SCN5A gene that affect sodium ion channels in the heart. This leads to abnormal depolarization and repolarization of cardiac cells, increasing the risk of:
- Ventricular arrhythmias
- Syncope (fainting)
- Sudden cardiac death
Brugada Syndrome is often asymptomatic until a serious arrhythmic event occurs, which makes early detection critical. It is more common in males and individuals of Asian descent, including Korean populations.
Symptoms
Symptoms may vary, and many individuals remain asymptomatic until adulthood. Key signs include:
- Syncope or fainting, often during sleep or at rest
- Palpitations due to abnormal heart rhythms
- Nocturnal agonal respiration (gasping during sleep)
- Sudden cardiac arrest, sometimes the first manifestation
- Seizure-like episodes caused by decreased blood flow to the brain during arrhythmias
- Fatigue or dizziness, particularly during febrile illnesses
Symptoms are often provoked by fever, certain medications, or electrolyte imbalances.
Causes
Brugada Syndrome is primarily genetic, but environmental and physiological factors can trigger arrhythmias:
- Mutations in the SCN5A gene, affecting sodium channels
- Other genetic mutations in genes regulating cardiac ion channels
- Fever, which can exacerbate ECG abnormalities
- Certain medications, including some antiarrhythmics, antidepressants, and anesthetics
- Electrolyte disturbances, such as low potassium or calcium levels
The interplay of genetic predisposition and triggers determines the risk and severity of arrhythmic events.
Risk Factors
- Family history of Brugada Syndrome or sudden cardiac death
- Male sex, particularly in adulthood
- Asian ethnicity, including Korean populations
- Fever or infections that increase arrhythmic risk
- Use of medications that affect cardiac conduction
- Underlying heart disease or structural abnormalities in rare cases
Complications
Brugada Syndrome can lead to life-threatening cardiac events, including:
- Sudden cardiac arrest, often occurring during sleep or at rest
- Ventricular fibrillation, a fatal arrhythmia if untreated
- Recurrent syncope, leading to injuries
- Psychological distress due to fear of sudden cardiac events
- Increased mortality risk without appropriate management
Prevention
Preventive strategies focus on reducing triggers and early detection:
- Avoid medications that prolong QT interval or affect sodium channels
- Prompt treatment of fever with antipyretics
- Regular ECG monitoring, particularly for individuals with family history
- Genetic counseling for high-risk families
- Lifestyle modifications, such as avoiding excessive alcohol and strenuous activity during illness
- Awareness of warning signs, such as unexplained fainting or palpitations
Treatment Options in Korea
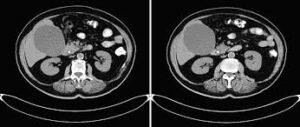
Diagnosis
Accurate diagnosis relies on clinical evaluation, ECG findings, and genetic testing:
- 12-lead ECG showing characteristic patterns, such as coved ST-segment elevation in leads V1–V3
- Holter monitoring for intermittent arrhythmias
- Electrophysiological studies to assess arrhythmic risk
- Genetic testing for SCN5A or related mutations
- Family screening in first-degree relatives
Medical Management
Treatment focuses on preventing arrhythmias and sudden cardiac death:
- Implantable cardioverter-defibrillator (ICD) placement in high-risk patients
- Medications such as quinidine to prevent ventricular arrhythmias in select cases
- Avoidance of arrhythmia-triggering drugs
- Fever management with antipyretics to prevent arrhythmia during infections
Lifestyle and Supportive Care
- Patient education about symptom recognition and emergency response
- Regular follow-ups with cardiologists for ECG monitoring and device checks
- Counseling and psychological support to manage anxiety related to cardiac risk
- Physical activity guidance to avoid high-risk situations without compromising overall health
Prognosis
The prognosis of Brugada Syndrome depends on early detection, risk stratification, and appropriate interventions:
- Asymptomatic individuals with Brugada ECG patterns may have a low risk of sudden cardiac death but require monitoring
- Patients with prior syncope or documented ventricular arrhythmias are at high risk and benefit from ICD implantation
- With advanced cardiac care in Korea, including electrophysiology units and genetic counseling, patients can reduce the risk of life-threatening events
- Ongoing follow-up and preventive strategies significantly improve survival and quality of life
Korean cardiology centers provide comprehensive care for Brugada Syndrome, including state-of-the-art diagnostics, arrhythmia management, patient education, and genetic counseling, ensuring optimal outcomes for affected individuals.