Overview
Botryomycosis is a rare, chronic bacterial infection affecting the skin, subcutaneous tissue, or internal organs, characterized by granulomatous lesions and slow-progressing nodules. Despite its name, botryomycosis is bacterial rather than fungal, most commonly caused by Staphylococcus aureus.
In Korea, botryomycosis is treated in dermatology and infectious disease centers, where early diagnosis, targeted antibiotic therapy, and surgical intervention are used to manage lesions and prevent complications. Due to its rarity, Korean hospitals often consult specialized microbiology and pathology departments for accurate identification and treatment planning.
What is Botryomycosis?
Botryomycosis is a chronic bacterial infection that produces granulomatous lesions resembling clusters of grapes, hence its name (from Greek “botrys,” meaning grape). The infection can be:
- Cutaneous: Affecting skin and subcutaneous tissue, often following trauma or injury
- Visceral: Rarely involving internal organs such as lungs, liver, or spleen
- Post-surgical: Can occur at surgical sites, especially in immunocompromised individuals
The disease progresses slowly over weeks to months, and untreated lesions can persist or expand.
Symptoms
Symptoms vary depending on location and severity:
- Cutaneous lesions: Firm nodules, abscesses, or ulcerated skin areas
- Discharge of pus: Often containing granules or bacterial colonies
- Slow progression: Lesions expand gradually over months
- Pain or tenderness at affected sites
- Fever or systemic symptoms may occur in visceral forms or secondary infections
- Scarring or tissue deformation in chronic cases
- Respiratory symptoms if lungs are involved (cough, shortness of breath)
Cutaneous botryomycosis is most common, while visceral forms are extremely rare and often more severe.
Causes
Botryomycosis is caused by bacterial infection, primarily:
- Staphylococcus aureus (most common)
- Pseudomonas aeruginosa
- Escherichia coli
- Other opportunistic bacteria in immunocompromised patients
Predisposing factors include:
- Skin trauma or wounds: Cuts, insect bites, burns, or surgical incisions
- Chronic diseases: Diabetes, vascular disorders, or immunodeficiency
- Surgical procedures: Especially if sterile techniques are compromised
- Underlying infections: Secondary infection of chronic wounds or ulcers
Risk Factors
- Immunocompromised status: HIV, chemotherapy, or long-term corticosteroid therapy
- Diabetes mellitus: Impaired wound healing increases susceptibility
- History of trauma or surgery
- Poor wound hygiene or chronic ulceration
- Chronic skin conditions that compromise the barrier function
- Occupational risk: Individuals with frequent skin injuries or exposure to bacteria
Complications
If untreated, botryomycosis can lead to serious complications:
- Chronic lesions with persistent pain or ulceration
- Secondary infections: Increased risk of sepsis if bacteria spread
- Scarring or deformity: Especially in visible skin areas
- Visceral involvement: Can damage internal organs, leading to respiratory, hepatic, or renal complications
- Delayed diagnosis: Misdiagnosis as fungal infection or tumor can delay appropriate therapy
Prevention
Preventive measures focus on infection control, wound care, and overall health:
- Prompt care of skin wounds or trauma
- Maintain proper hygiene to reduce bacterial exposure
- Monitor chronic ulcers or surgical sites for early signs of infection
- Manage underlying conditions such as diabetes or immunodeficiency
- Protective clothing and gloves in occupational or high-risk settings
- Regular medical follow-up for individuals with chronic wounds or post-surgical sites
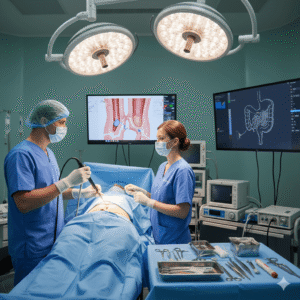
Treatment Options in Korea
Diagnosis
Accurate diagnosis is essential due to the rarity of botryomycosis:
- Clinical examination: Assessment of nodules, ulcers, or abscesses
- Microbiological culture: Identification of causative bacteria from lesion samples
- Histopathology: Granulomatous tissue evaluation, often showing bacterial colonies in eosinophilic material
- Imaging: Ultrasound, CT, or MRI for deeper tissue involvement or visceral disease
- Blood tests: Evaluate infection markers, especially in systemic cases
Medical Management
- Targeted antibiotics: Based on culture and sensitivity results; commonly used antibiotics include cephalosporins, vancomycin, or combination therapy for resistant strains
- Long-term therapy: Several weeks to months may be required for complete resolution
- Pain management: Analgesics to reduce discomfort from lesions
- Adjunctive care: Dressings, antiseptic applications, and wound hygiene
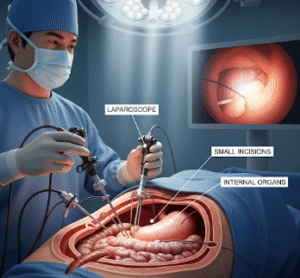
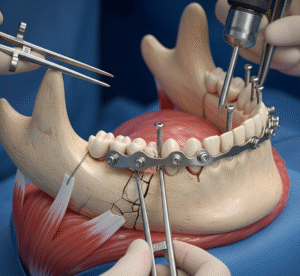
Surgical Management
Surgery is indicated in cases where:
- Lesions are extensive or non-responsive to antibiotics
- Abscesses require drainage
- Scarring or deformity is present
- Procedures include excision of nodules, debridement of infected tissue, and reconstruction if necessary
Korean surgical centers emphasize minimally invasive techniques and precision debridement, reducing recovery time and preserving tissue integrity.
Supportive Care
- Regular follow-up: Monitor for recurrence or complications
- Nutrition: Adequate protein and vitamins support immune function and tissue repair
- Psychological support: Chronic infections can impact mental well-being
- Infection control measures: Prevent secondary infections during recovery
Prognosis
The prognosis for botryomycosis in Korea is generally favorable with timely diagnosis and proper treatment:
- Cutaneous lesions respond well to antibiotics and surgery, often with complete resolution
- Visceral or systemic forms may require more aggressive therapy but can be managed successfully in specialized centers
- Early intervention reduces the risk of scarring, tissue damage, and systemic complications
- Follow-up care ensures early detection of recurrence or secondary infections
Korean hospitals provide advanced diagnostic tools, culture-based targeted therapy, and surgical expertise, offering patients excellent outcomes and recovery support.