Overview
Type 1 Diabetes (T1D) is a chronic autoimmune condition in which the body’s immune system attacks and destroys insulin-producing beta cells in the pancreas. Unlike Type 2 diabetes, which is often linked to lifestyle factors, T1D typically develops in children, adolescents, or young adults, although it can occur at any age. Insulin deficiency leads to elevated blood glucose levels, causing a wide range of metabolic disturbances. South Korea offers advanced endocrinology services, continuous glucose monitoring systems, insulin therapies, and specialized diabetes education programs to manage T1D effectively and reduce long-term complications.
What is Type 1 Diabetes?
Type 1 Diabetes is an autoimmune disease characterized by the destruction of pancreatic beta cells, resulting in absolute insulin deficiency. Insulin is essential for transporting glucose from the bloodstream into cells for energy. Without insulin, blood glucose rises, leading to hyperglycemia and potential acute and chronic complications. T1D can be classified into:
- Autoimmune T1D: Most common form, caused by immune-mediated beta-cell destruction
- Idiopathic T1D: Rare form without evidence of autoimmunity, with similar clinical manifestations
In South Korea, early diagnosis through blood glucose testing, C-peptide measurement, and autoantibody screening allows timely initiation of insulin therapy and metabolic control.
Symptoms
Symptoms of Type 1 Diabetes often develop rapidly over days to weeks and include:
- Increased thirst (polydipsia) and frequent urination (polyuria)
- Unexplained weight loss despite normal or increased appetite
- Fatigue and weakness due to inability to utilize glucose for energy
- Blurred vision from changes in blood sugar levels
- Nausea, vomiting, or abdominal pain in cases of diabetic ketoacidosis
- Rapid breathing, fruity-smelling breath, or confusion in severe cases
Early recognition of these symptoms is critical in South Korea, where immediate medical care can prevent life-threatening complications such as diabetic ketoacidosis.
Causes
Type 1 Diabetes is primarily caused by autoimmune destruction of pancreatic beta cells, but the exact trigger is multifactorial:
- Genetic predisposition: Certain HLA genotypes increase susceptibility
- Autoimmune factors: Presence of autoantibodies against pancreatic cells
- Environmental triggers: Viral infections, early-life dietary factors, or unknown environmental exposures may initiate autoimmune reactions
- Immune dysregulation: Dysfunction of T-cells or regulatory mechanisms leading to beta-cell attack
South Korean research centers monitor genetic and environmental factors contributing to T1D to improve early detection and preventive strategies.
Risk Factors
Key risk factors for T1D include:
- Family history of Type 1 Diabetes or other autoimmune disorders
- Specific HLA gene variants associated with autoimmune susceptibility
- Personal history of autoimmune diseases such as thyroiditis or celiac disease
- Viral infections during early childhood, including enteroviruses or rubella
In South Korea, children with high-risk genetic profiles are often monitored closely for early signs of T1D, including autoantibody testing and glucose monitoring.
Complications
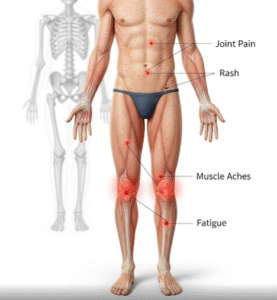
Without proper management, Type 1 Diabetes can lead to acute and chronic complications:
- Acute complications:
- Diabetic ketoacidosis, a life-threatening condition caused by severe insulin deficiency
- Hypoglycemia due to insulin overdose or missed meals
- Chronic complications:
- Cardiovascular disease, including heart attacks and strokes
- Kidney disease (diabetic nephropathy) leading to renal failure
- Nerve damage (diabetic neuropathy) causing pain, numbness, or foot ulcers
- Eye problems (diabetic retinopathy) potentially leading to blindness
- Skin infections and delayed wound healing
Regular follow-up and advanced diabetes care in South Korea reduce these risks and improve long-term outcomes for T1D patients.
Prevention
While Type 1 Diabetes cannot currently be prevented, early detection and intervention reduce the risk of acute complications:
- Genetic and antibody screening: For high-risk children and families
- Education: Recognizing early signs and symptoms of hyperglycemia or ketoacidosis
- Healthy lifestyle: Balanced diet, regular exercise, and infection control to support metabolic stability
- Vaccination: Protection against viral infections that may trigger autoimmune responses
South Korean pediatric endocrinology programs emphasize awareness, early diagnosis, and preventive monitoring in high-risk populations.
Treatment Options in Korea
Management of Type 1 Diabetes in South Korea focuses on lifelong insulin therapy, glucose monitoring, and multidisciplinary care:
Diagnosis:
- Blood glucose testing (fasting, random, and oral glucose tolerance tests)
- Measurement of C-peptide levels to assess endogenous insulin production
- Screening for islet autoantibodies (GAD, IA-2, insulin autoantibodies)
- Continuous monitoring of HbA1c levels to assess long-term glucose control
Medical Treatments:
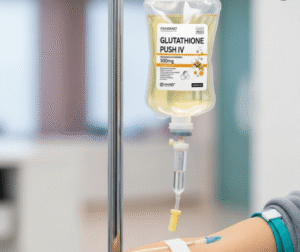
- Insulin therapy: Multiple daily injections or continuous subcutaneous insulin infusion (insulin pump)
- Continuous glucose monitoring (CGM): Real-time tracking of blood glucose for better management
- Adjunctive therapies: Medications to reduce cardiovascular or renal risk factors when indicated
Lifestyle and Supportive Care:
- Nutrition counseling to maintain optimal blood glucose levels
- Exercise guidance tailored to prevent hypoglycemia
- Education on recognizing and managing hypo- and hyperglycemia
- Psychological support to cope with chronic disease management
Advanced Interventions:
- Islet cell transplantation and immunomodulatory research are ongoing in South Korea, aiming to restore endogenous insulin production
- Telemedicine programs provide continuous follow-up and support for patients in remote areas
South Korea’s comprehensive diabetes care integrates endocrinology, nutrition, psychology, and technology to optimize management and improve the quality of life for individuals with Type 1 Diabetes.