Overview
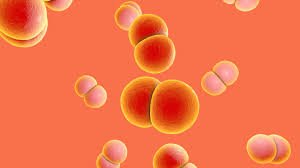
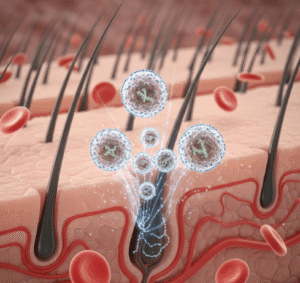
Tinea versicolor is a common superficial fungal infection of the skin caused by the yeast Malassezia, which naturally resides on the skin’s surface. This condition is characterized by patches of discolored skin, typically on the trunk, neck, and upper arms. While it is not life-threatening, tinea versicolor can cause cosmetic concerns, itching, and social discomfort. South Korea offers advanced dermatological care, including accurate diagnosis with Wood’s lamp examination, fungal culture, and dermoscopy, along with effective topical and systemic treatments to manage the condition and prevent recurrence.
What is Tinea Versicolor?
Tinea versicolor, also known as pityriasis versicolor, occurs when the Malassezia yeast overgrows and disrupts the natural pigmentation of the skin. This imbalance leads to small, scaly patches that may appear lighter or darker than the surrounding skin. The infection is more noticeable after sun exposure, as affected areas do not tan. It is a superficial infection affecting the outermost layer of the skin and typically does not penetrate deeper tissues or cause systemic illness. The condition can affect people of all ages but is more common in adolescents and young adults living in warm, humid environments.
Symptoms
The symptoms of tinea versicolor primarily involve changes in skin appearance and mild discomfort:
- Discolored patches: Light, dark, pink, or tan areas on the skin
- Fine scaling: Slight peeling or flaky texture on the affected patches
- Itching: Mild to moderate itching, especially in hot or humid conditions
- Spread and recurrence: Patches may merge or recur, particularly in warm climates
- Cosmetic impact: Noticeable discoloration may affect self-esteem and confidence
The most commonly affected areas include the chest, back, shoulders, neck, and upper arms. Although the infection is generally painless, the aesthetic changes often prompt patients to seek treatment.
Causes
Tinea versicolor results from the overgrowth of Malassezia yeast on the skin. Several factors can trigger or exacerbate the condition:
- Hot and humid weather: Promotes yeast proliferation
- Excessive sweating: Creates a moist environment conducive to fungal growth
- Oily skin: Sebum-rich areas support yeast overgrowth
- Weakened immune system: Makes the skin more susceptible to fungal imbalance
- Genetic predisposition: Family history may increase susceptibility
- Hormonal changes: Puberty or other hormonal fluctuations may trigger outbreaks
- Inadequate skin hygiene: Rarely, poor hygiene can contribute to yeast overgrowth
Risk Factors
Certain individuals are more prone to developing tinea versicolor:
- Adolescents and young adults with active sebaceous glands
- Residents of tropical or subtropical climates
- Individuals with hyperhidrosis (excessive sweating)
- People with compromised immunity due to medications or chronic conditions
- Those with oily skin or existing dermatological conditions
Complications
Tinea versicolor is generally benign but can lead to complications in some cases:
- Persistent or recurrent infection: Despite treatment, some individuals experience repeated outbreaks
- Cosmetic concerns: Discolored patches may persist even after the infection is cleared, affecting self-esteem
- Secondary bacterial infection: Scratching or irritation of the patches can lead to bacterial superinfection
- Delayed treatment impact: In rare cases, untreated infections may cover large areas, making management more challenging
Early diagnosis and treatment in Korea’s dermatology clinics help prevent prolonged cosmetic and psychological impacts.
Prevention
Preventing tinea versicolor focuses on reducing conditions that favor yeast overgrowth:
- Maintain dry, clean skin, especially in humid or sweaty conditions
- Use antifungal or medicated cleansers during hot, humid seasons
- Wear breathable clothing to reduce moisture accumulation
- Limit excessive use of oily skincare products on affected areas
- Promptly treat initial outbreaks to prevent recurrence
- Maintain overall immune health through proper nutrition, hydration, and stress management
Treatment Options in Korea
South Korea offers a variety of effective treatments for tinea versicolor, ranging from topical agents to systemic therapy for more extensive cases.
Diagnosis:
- Physical examination by a dermatologist
- Wood’s lamp examination to detect fluorescent patches under ultraviolet light
- Skin scraping for microscopic analysis or fungal culture
- Dermoscopy for precise assessment of lesion extent
Medical Treatments:
- Topical antifungal medications: Creams, lotions, or shampoos containing ketoconazole, selenium sulfide, clotrimazole, or terbinafine
- Oral antifungal medications: Fluconazole or itraconazole for severe, extensive, or recurrent cases
- Adjunct therapy: Mild corticosteroids may be used temporarily to reduce inflammation and itching
Rehabilitation and Support:
- Regular follow-up to monitor treatment response and recurrence
- Guidance on preventive measures, including hygiene and skin care routines
- Education on lifestyle modifications to minimize triggers such as heat, humidity, and sweating
- Counseling for patients concerned about cosmetic appearance or psychological impact
Korean dermatologists combine evidence-based pharmacological therapy with patient education and preventive strategies to ensure effective management and long-term control of tinea versicolor. Most patients experience significant improvement within weeks, and recurrence can be minimized with proper preventive care.