Overview
Transverse Myelitis (TM) is a rare neurological disorder characterized by inflammation of the spinal cord, leading to motor, sensory, and autonomic dysfunction. It can affect any age group and may occur as a primary condition or secondary to infections, autoimmune diseases, or multiple sclerosis. The condition often develops rapidly, causing weakness, sensory disturbances, and in severe cases, paralysis. South Korea offers advanced diagnostic imaging, immunotherapy, and rehabilitation programs for TM, providing multidisciplinary care to reduce neurological deficits, manage symptoms, and improve patients’ quality of life.
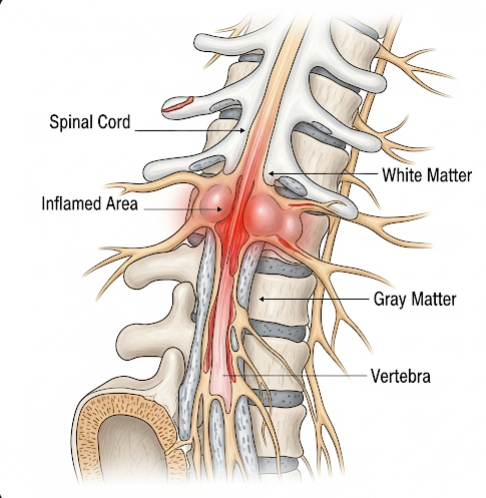
What is Transverse Myelitis?
Transverse Myelitis is an inflammatory process that affects a segment of the spinal cord across its width, disrupting communication between the brain and the rest of the body. The inflammation can damage myelin—the protective covering of nerve fibers—leading to motor weakness, sensory changes, and autonomic dysfunction such as bladder and bowel problems. TM may occur idiopathically, post-infection, or in association with autoimmune disorders such as systemic lupus erythematosus or multiple sclerosis. Early recognition and intervention in Korean neurology centers are crucial for limiting long-term disability and optimizing recovery.
Symptoms
Symptoms of Transverse Myelitis develop over hours to days and may vary depending on the affected spinal cord segment:
- Motor symptoms: Weakness in the legs, arms, or trunk; in severe cases, paralysis
- Sensory symptoms: Tingling, numbness, burning sensations, or loss of sensation below the level of inflammation
- Pain: Localized back pain or radicular pain radiating to the limbs
- Autonomic dysfunction: Bladder retention, urinary urgency, bowel dysfunction, or sexual dysfunction
- Spasticity: Muscle stiffness and involuntary spasms
- Fatigue and malaise: General feeling of weakness or discomfort
- Rapid symptom progression: Symptoms may worsen over hours or days, requiring urgent medical attention
Prompt evaluation in South Korean hospitals enables early treatment and reduces the risk of permanent neurological deficits.
Causes
Transverse Myelitis can result from various triggers, though the exact cause is often idiopathic:
- Infections: Viral, bacterial, or parasitic infections can trigger immune-mediated spinal inflammation
- Autoimmune disorders: Multiple sclerosis, neuromyelitis optica, systemic lupus erythematosus, or sarcoidosis
- Vaccinations: Rarely, post-vaccination immune responses have been implicated
- Idiopathic: In many cases, no identifiable cause is found
- Other inflammatory conditions: Vasculitis or post-infectious syndromes
The inflammation damages spinal cord tissue and disrupts nerve signal transmission, leading to the characteristic neurological deficits of TM.
Risk Factors
Certain factors may increase the likelihood of developing Transverse Myelitis:
- Recent viral or bacterial infection
- Autoimmune or inflammatory disorders
- Family history of multiple sclerosis or other demyelinating diseases
- Younger age in children or young adults; a second peak may occur in middle-aged adults
- History of vaccination or immune system modulation in rare cases
Identifying risk factors aids Korean neurologists in early diagnosis and personalized management strategies.
Complications
Transverse Myelitis can lead to significant complications if not treated promptly:
- Paralysis: Partial or complete loss of motor function below the affected spinal cord segment
- Permanent sensory deficits: Persistent numbness or altered sensation
- Bladder and bowel dysfunction: Long-term urinary retention or incontinence
- Spasticity and muscle contractures: Leading to mobility limitations
- Chronic pain: Neuropathic pain caused by nerve damage
- Secondary complications: Pressure sores, infections, and reduced mobility-related issues
- Psychological impact: Depression, anxiety, and decreased quality of life due to functional limitations
Early treatment in Korea mitigates these risks and promotes neurological recovery.
Prevention
While idiopathic cases cannot be entirely prevented, certain measures reduce risk or severity:
- Prompt treatment of infections to prevent post-infectious inflammation
- Management of autoimmune or inflammatory disorders with appropriate medications
- Awareness of early neurological symptoms and seeking immediate medical attention
- Maintaining general health and immune system support through nutrition, exercise, and stress management
Public health awareness and patient education in Korea help facilitate early recognition and reduce long-term complications.
Treatment Options in Korea
South Korea provides multidisciplinary care for Transverse Myelitis, combining neurology, rehabilitation, and supportive therapies:
Diagnosis:
- MRI of the spinal cord to identify inflammation and segment involvement
- Blood tests for autoimmune markers, infections, and inflammatory indicators
- Cerebrospinal fluid (CSF) analysis to detect inflammatory cells or antibodies
- Electrophysiological studies to assess nerve conduction and spinal cord function
- Comprehensive neurological evaluation for motor, sensory, and autonomic function
Medical Treatments:
- High-dose corticosteroids: Reduce inflammation and limit spinal cord damage
- Plasma exchange (plasmapheresis): Used in severe or steroid-resistant cases
- Intravenous immunoglobulin (IVIG): Modulates immune response in selected patients
- Pain management: Medications for neuropathic or musculoskeletal pain
- Treatment of underlying causes: Antivirals, antibiotics, or immunosuppressive therapy if secondary to infection or autoimmune disease
Rehabilitation and Support:
- Physical therapy to improve mobility, strength, and coordination
- Occupational therapy to enhance daily living activities and independence
- Bladder and bowel management programs for autonomic dysfunction
- Psychological support to address depression, anxiety, and coping strategies
- Long-term follow-up for monitoring disease progression and preventing relapse
Korean neurology centers integrate early intervention, advanced immunotherapy, and comprehensive rehabilitation to optimize recovery and support functional independence for patients with Transverse Myelitis.