Overview
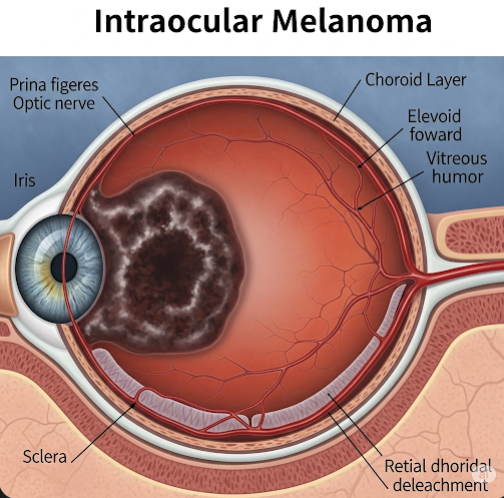
Intraocular melanoma, also known as uveal melanoma, is the most common primary eye cancer in adults, originating from melanocytes within the uveal tract of the eye. The uveal tract comprises three main parts: the iris (colored part of the eye), the ciliary body (responsible for aqueous humor production), and the choroid (vascular layer beneath the retina). Though relatively rare, intraocular melanoma is a serious condition because it can cause significant vision loss and has the potential to metastasize to distant organs, particularly the liver. The prognosis depends heavily on early detection and effective treatment. In Korea, patients benefit from sophisticated diagnostic tools, experienced ocular oncologists, and access to advanced treatments that prioritize both tumor control and vision preservation.
What is Intraocular Melanoma?
Intraocular melanoma arises from the malignant transformation of melanocytes — pigment-producing cells responsible for eye color — within the uveal tract. It is histologically similar to cutaneous melanoma but differs in clinical behavior, treatment, and metastatic pattern.
The tumor can originate in different parts of the uvea:
- Choroidal melanoma: The most common form (~85%), developing in the choroid layer beneath the retina. It often presents as a dome-shaped mass visible during retinal examination.
- Ciliary body melanoma: Occurs in the ciliary body and may be harder to detect early, as symptoms often appear later.
- Iris melanoma: Least common (~4%), typically diagnosed earlier because of visible changes in iris color or shape.
Intraocular melanomas tend to grow slowly but can invade adjacent ocular tissues and spread via blood vessels to other body parts. Unlike skin melanoma, lymphatic spread is rare due to the eye’s lack of lymphatics.
Symptoms
Early stages of intraocular melanoma are often asymptomatic, making routine eye exams critical. Symptoms generally appear as the tumor enlarges or disrupts normal eye function:
- Visual disturbances: Blurred vision, decreased visual acuity, or sudden vision loss.
- Floaters: Perceived as spots or shadows drifting across the field of vision, caused by tumor-related vitreous changes.
- Photopsia: Flashes of light due to retinal irritation.
- Visual field defects: Partial loss of peripheral or central vision, depending on tumor location.
- Change in iris appearance: New pigmentation, mass, or distortion of the pupil if the iris is involved.
- Eye redness or pain: Usually late symptoms, possibly indicating secondary glaucoma or inflammation.
- Proptosis (bulging eye): Occurs with large tumors extending beyond the globe.
Many patients discover intraocular melanoma incidentally during routine ophthalmic screenings.
Causes
The exact causes of intraocular melanoma are not fully elucidated but involve genetic and environmental factors:
- Genetic mutations: Somatic mutations in genes such as GNAQ, GNA11, BAP1, SF3B1, and EIF1AX have been identified in tumor cells and influence tumor behavior and prognosis.
- Ultraviolet (UV) light exposure: Unlike skin melanoma, the link between UV exposure and uveal melanoma is weaker, but some studies suggest cumulative UV radiation may contribute.
- Pigmentation: Light-colored irides (blue or green eyes) lack protective melanin, increasing vulnerability to malignant transformation.
- Age and ethnicity: Most patients are middle-aged or older adults; uveal melanoma is rare in Asian populations, including Koreans, and more prevalent in Caucasians.
- Ocular conditions: Presence of ocular or oculodermal melanocytosis (increased pigmentation in the eye or surrounding skin) raises risk.
- Family history: A history of melanoma or other cancers increases susceptibility.
Risk Factors
Risk factors for developing intraocular melanoma include:
- Light eye color: Blue, green, or gray eyes confer increased risk due to less melanin protection.
- Fair skin and inability to tan well.
- Presence of atypical melanocytic lesions in the eye.
- Genetic predisposition: Hereditary cancer syndromes involving BAP1 mutations.
- Age: Typically diagnosed between 50-70 years of age.
- Certain environmental exposures: Though evidence is limited, chronic exposure to welding arcs or UV radiation may play a role.
Complications
Without timely diagnosis and treatment, intraocular melanoma can lead to:
- Vision loss: Tumor growth can cause retinal detachment, cataracts, or optic nerve damage, leading to partial or complete blindness.
- Secondary glaucoma: Tumor invasion can block aqueous humor outflow, increasing intraocular pressure and causing painful glaucoma.
- Retinal detachment: Fluid accumulation separates the retina, resulting in vision deterioration.
- Extraocular extension: Tumor may invade surrounding tissues, including orbit or brain, worsening prognosis.
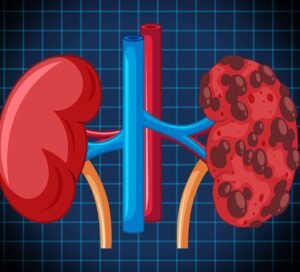
- Metastasis: Hematogenous spread primarily targets the liver (up to 90% of metastatic cases), followed by lungs, bone, and skin. Liver metastases are often fatal and difficult to treat.
- Enucleation: In advanced cases or when other treatments fail, surgical removal of the eye is necessary.
Prevention
Although no guaranteed prevention exists, certain measures may reduce risk or enable early detection:
- Regular comprehensive eye exams: Especially for individuals with risk factors or suspicious pigmented lesions.
- UV protection: Wearing sunglasses with 100% UV blocking to protect ocular tissues from UV damage.
- Awareness of changes: Prompt ophthalmologic evaluation for any visual changes, eye pain, or visible iris abnormalities.
- Genetic counseling: For families with hereditary melanoma syndromes.
Treatment Options in Korea
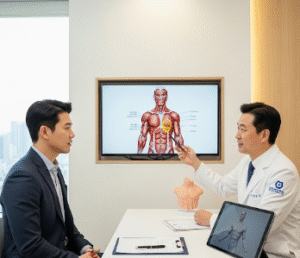
Korea’s ophthalmology and oncology centers provide cutting-edge, multidisciplinary care for intraocular melanoma:
- Diagnostic Workup:
- Detailed ophthalmologic exam: Slit-lamp biomicroscopy and indirect ophthalmoscopy to evaluate tumor characteristics.
- Ultrasound biomicroscopy (UBM) and ocular ultrasound: To assess tumor size, shape, internal reflectivity, and ciliary body involvement.
- Optical coherence tomography (OCT): High-resolution imaging of retinal and choroidal layers affected by tumor.
- Fluorescein and indocyanine green angiography: To study tumor vascularity and leakage.
- Fine-needle aspiration biopsy: Performed in selected cases for cytological diagnosis and genetic profiling.
- Treatment Modalities:
- Plaque brachytherapy: Placement of a radioactive plaque on the sclera overlying the tumor delivers targeted radiation, aiming to eradicate the tumor while preserving the eye and vision.
- Proton beam therapy: Precise external radiation using proton particles, minimizing damage to surrounding tissues, effective for larger or difficult-to-access tumors.
- Local resection (eye-sparing surgery): Surgical removal of the tumor with reconstruction, mainly for small, accessible tumors.
- Enucleation: Complete removal of the eye for large tumors, extensive involvement, or when vision preservation is impossible.
- Laser photocoagulation or transpupillary thermotherapy: Adjunctive treatments in select cases.
- Systemic Monitoring:
- Regular surveillance for metastasis, focusing on liver function tests and imaging (ultrasound, CT, or MRI).
- In cases of metastasis, systemic treatments such as chemotherapy, immunotherapy (e.g., immune checkpoint inhibitors), targeted therapy, or enrollment in clinical trials may be offered.
- Multidisciplinary Team:
- Korean centers coordinate care among ophthalmologists, radiation oncologists, medical oncologists, genetic counselors, and specialized nursing staff to ensure comprehensive patient management.
- Research and Innovation:
- Korea participates in ongoing research into genetic markers, novel therapies, and improved diagnostic tools to enhance outcomes for intraocular melanoma patients.