Overview
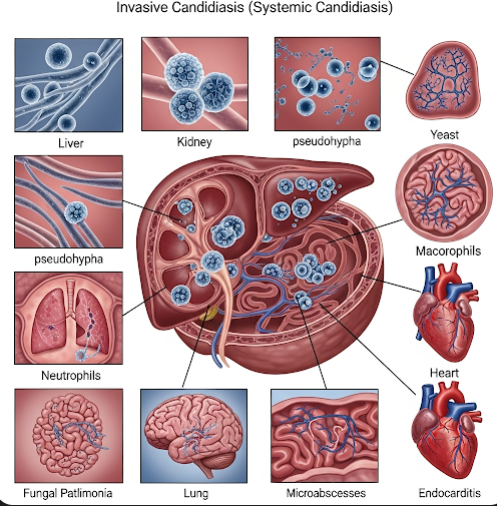
Invasive candidiasis, also known as systemic candidiasis, is a serious fungal infection caused by Candida species entering the bloodstream or deep tissues, leading to widespread infection. Unlike superficial Candida infections affecting the skin or mucous membranes, invasive candidiasis affects internal organs and the bloodstream, posing significant risk especially in immunocompromised individuals or patients with medical devices. It is a leading cause of fungal sepsis worldwide and is associated with high morbidity and mortality if not promptly diagnosed and treated. In Korea, advanced diagnostic methods, antifungal therapies, and specialized infectious disease care improve outcomes for patients with invasive candidiasis.
What is Invasive Candidiasis?
Invasive candidiasis occurs when Candida fungi, normally harmless commensals found on the skin, mouth, gastrointestinal tract, and genitals, penetrate the body’s barriers and enter sterile sites such as the bloodstream (candidemia) or internal organs (deep-seated candidiasis). The infection can involve multiple organs including the heart (endocarditis), kidneys, liver, spleen, eyes (endophthalmitis), and central nervous system.
Candida albicans is the most common species causing invasive disease, but non-albicans species such as Candida glabrata, Candida tropicalis, Candida parapsilosis, and Candida krusei are increasingly recognized and often show varying antifungal resistance patterns.
Symptoms
Symptoms of invasive candidiasis can be nonspecific and depend on the site and severity of infection:
- Fever and chills that do not improve with antibiotics.
- Sepsis or septic shock: Low blood pressure, rapid heartbeat, confusion, and organ dysfunction.
- General malaise, fatigue, and weakness.
- Symptoms related to organ involvement:
- Kidneys: Flank pain, abnormal urine.
- Eyes: Visual disturbances if endophthalmitis develops.
- Heart: Signs of endocarditis such as new heart murmur.
- Lungs: Cough or respiratory distress.
- Laboratory abnormalities: Elevated inflammatory markers, positive blood cultures for Candida.
Causes
Invasive candidiasis usually occurs when the normal barriers to Candida invasion are disrupted or the immune system is weakened. Factors that facilitate Candida entry and proliferation include:
- Compromised immune system: Due to HIV/AIDS, cancer chemotherapy, organ transplantation, or corticosteroid use.
- Broad-spectrum antibiotic use: Disrupts normal bacterial flora that suppress Candida growth.
- Central venous catheters or other invasive devices: Provide a direct route for Candida to enter the bloodstream.
- Prolonged hospitalization and ICU stay.
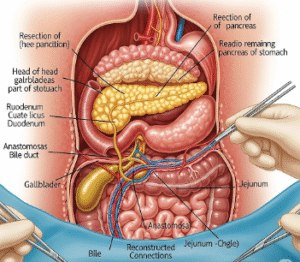
- Surgery, especially abdominal or gastrointestinal.
- Diabetes mellitus or other chronic diseases.
- Total parenteral nutrition (TPN).
Risk Factors
- Critical illness or intensive care admission.
- Immunosuppression: Chemotherapy, organ transplant, HIV infection.
- Use of broad-spectrum antibiotics.
- Presence of intravascular devices: Central lines, urinary catheters.
- Recent surgery or trauma.
- Prematurity or low birth weight in neonates.
- Diabetes mellitus and other chronic illnesses.
Complications
If untreated or inadequately treated, invasive candidiasis can cause severe complications:
- Disseminated infection: Multi-organ failure due to fungal spread.
- Endocarditis: Infection of heart valves requiring prolonged therapy or surgery.
- Endophthalmitis: Fungal infection of the eye leading to vision loss.
- Renal failure: Due to kidney involvement.
- Septic shock and death: High mortality especially in critically ill patients.
- Recurrence or persistent infection: May occur if source control is inadequate.
Prevention
Preventive measures are critical, especially in high-risk patients:
- Strict infection control and hand hygiene in hospitals.
- Careful use and early removal of invasive devices like central lines.
- Antifungal prophylaxis in high-risk patients as per guidelines.
- Antibiotic stewardship to minimize unnecessary broad-spectrum antibiotic use.
- Prompt treatment of localized Candida infections to prevent dissemination.
- Regular monitoring in ICU patients and immunocompromised individuals.
Treatment Options in Korea
Korea offers advanced care for invasive candidiasis with a combination of rapid diagnostics and effective antifungal therapies:
- Diagnostic Approaches:
- Blood cultures: Standard for detecting candidemia but can be slow and insensitive.
- Non-culture diagnostics: Beta-D-glucan assay, PCR-based tests, and T2Candida panel provide faster and more sensitive detection.
- Imaging: To identify organ involvement.
- Ophthalmologic exam: To screen for ocular involvement.
- Antifungal Therapy:
- Echinocandins (e.g., caspofungin, micafungin): First-line agents due to efficacy and safety.
- Azoles (fluconazole, voriconazole): Used based on susceptibility and patient condition.
- Amphotericin B: Reserved for resistant infections or severe cases.
- Duration: Typically 2 weeks after clearance of Candida from blood and resolution of symptoms.
- Source control: Removal of infected catheters or devices is essential.
- Supportive Care:
- Management of sepsis, organ support in ICU.
- Monitoring and managing complications.
- Multidisciplinary Management:
- Infectious disease specialists, critical care teams, microbiologists, and pharmacists collaborate for personalized treatment plans.