Overview
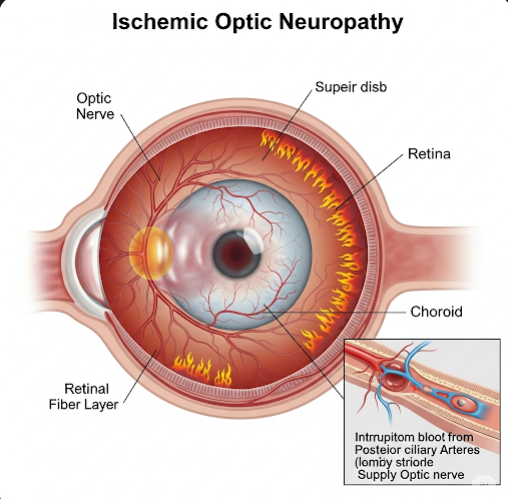
Ischemic optic neuropathy (ION) is a serious eye condition caused by insufficient blood flow to the optic nerve, which can result in sudden, painless vision loss. The optic nerve is vital for transmitting visual information from the retina to the brain, and damage due to ischemia can lead to permanent visual impairment or blindness if not promptly recognized and treated. ION is one of the leading causes of acute optic nerve-related vision loss, particularly in older adults. It is broadly classified into two types: anterior ischemic optic neuropathy (AION), affecting the optic nerve head at the front of the nerve, and posterior ischemic optic neuropathy (PION), involving the portion of the optic nerve behind the eye. In Korea, timely diagnosis and multidisciplinary management involving ophthalmologists, neurologists, and rheumatologists help optimize patient outcomes.
What is Ischemic Optic Neuropathy?
Ischemic optic neuropathy occurs when the blood supply to the optic nerve is compromised, causing ischemia and resulting in injury or death of the nerve fibers. The optic nerve head receives blood from small branches of the posterior ciliary arteries, which can be obstructed or narrowed by vascular disease, inflammation, or other factors. This ischemia disrupts nerve function, producing visual symptoms.
- Anterior Ischemic Optic Neuropathy (AION): The more common form, typically visible as swelling of the optic disc on fundoscopy.
- Posterior Ischemic Optic Neuropathy (PION): Rarer and more challenging to diagnose early because the optic disc appears normal initially but later develops atrophy.
Symptoms
The onset of ischemic optic neuropathy is usually sudden and painless. Typical symptoms include:
- Sudden vision loss: Usually in one eye, ranging from mild blurring to complete loss of vision.
- Visual field defects: Most commonly altitudinal defects, meaning loss of the upper or lower half of the visual field.
- Color vision changes: Diminished color perception or contrast sensitivity.
- Optic disc swelling: Seen in AION during eye examination; PION initially shows a normal optic disc.
- No significant pain: Unlike optic neuritis, pain is uncommon or mild.
- Possible transient vision disturbances: Brief episodes of vision loss (amaurosis fugax) can precede the event.
Causes
Ischemic optic neuropathy arises primarily due to impaired blood flow to the optic nerve from various causes:
- Non-arteritic anterior ischemic optic neuropathy (NAION): The most common type, linked to small vessel disease and vascular risk factors such as hypertension and diabetes. It often occurs in patients with a structurally small optic disc (“disc at risk”) predisposing to circulatory compromise.
- Arteritic anterior ischemic optic neuropathy: Caused by giant cell arteritis (GCA), a systemic vasculitis affecting medium and large arteries, including the posterior ciliary arteries. This form is more severe and requires urgent corticosteroid treatment to prevent blindness.
- Systemic hypotension: Excessive drops in blood pressure, especially nocturnal hypotension, may precipitate ischemia.
- Atherosclerosis: Narrowing or occlusion of vessels supplying the optic nerve.
- Embolic events or thrombosis: Blocking the optic nerve’s blood supply.
- Perioperative causes: Hypotension, anemia, or prolonged surgery can cause PION.
- Other vasculopathies: Including vasculitis, autoimmune diseases, or hypercoagulable states.
Risk Factors
- Age: Most patients are over 50 years, with increasing risk with age.
- Vascular diseases: Hypertension, diabetes mellitus, hyperlipidemia.
- Smoking: Accelerates vascular damage.
- Sleep apnea: Associated with nocturnal hypoxia and hypotension.
- Anatomical predisposition: Small optic nerve heads increase risk.
- Giant cell arteritis: Especially in patients over 70 years.
- Medications: Some blood pressure-lowering drugs may contribute by causing nocturnal hypotension.
- Other systemic conditions: Atrial fibrillation, carotid artery disease.
Complications
- Permanent vision loss: Partial or complete in the affected eye, often irreversible.
- Visual field defects: Affecting daily functioning, such as reading or driving.
- Contralateral eye involvement: Risk of the second eye being affected, particularly in arteritic AION without treatment.
- Optic nerve atrophy: Visible on fundoscopic examination weeks to months after the event, indicating nerve fiber loss.
- Psychological impact: Sudden vision loss can lead to anxiety, depression, or reduced quality of life.
- Blindness: In severe or untreated arteritic AION cases.
Prevention
Prevention strategies focus on identifying and controlling modifiable risk factors:
- Manage cardiovascular health: Control hypertension, diabetes, and cholesterol levels rigorously.
- Smoking cessation: To reduce vascular damage and improve circulation.
- Treatment of sleep apnea: Reduces nocturnal hypoxia and hypotension.
- Avoid excessive nocturnal hypotension: Adjust antihypertensive medication timing and dosage.
- Early diagnosis and treatment of giant cell arteritis: Prompt corticosteroid therapy can prevent bilateral blindness.
- Regular ophthalmic examinations: Especially in high-risk individuals for early detection of changes.
- Patient education: Awareness of symptoms to seek immediate medical attention.
Treatment Options in Korea
In Korea, the management of ischemic optic neuropathy involves a coordinated approach by ophthalmologists, neurologists, and other specialists:
- Diagnostic evaluation:
- Comprehensive eye examination: Visual acuity, color vision, and detailed fundoscopic examination to detect optic disc swelling or pallor.
- Visual field testing: To characterize the pattern and extent of vision loss.
- Optical coherence tomography (OCT): Imaging to assess optic nerve fiber layer thickness and damage.
- Fluorescein angiography: To evaluate optic nerve head perfusion in some cases.
- Laboratory testing: ESR, CRP, and temporal artery biopsy to diagnose giant cell arteritis in suspected arteritic AION.
- Neuroimaging: MRI to exclude other causes of optic neuropathy.
- Medical management:
- Non-arteritic AION: No proven effective treatment to reverse vision loss; management focuses on controlling vascular risk factors and preventing involvement of the other eye.
- Arteritic AION: High-dose systemic corticosteroids are started immediately to halt disease progression and prevent vision loss in the fellow eye.
- Adjunct therapies: Control of comorbidities like hypertension, diabetes, and sleep apnea.
- Monitoring and follow-up: Regular ophthalmic evaluations to assess for progression or complications.
- Supportive care:
- Visual rehabilitation and aids to help patients adapt to vision loss.
- Psychological support and counseling.
- Research and emerging treatments: Korea actively participates in clinical research exploring neuroprotective agents and therapies aimed at optic nerve regeneration, though no definitive treatments are currently available.