Overview
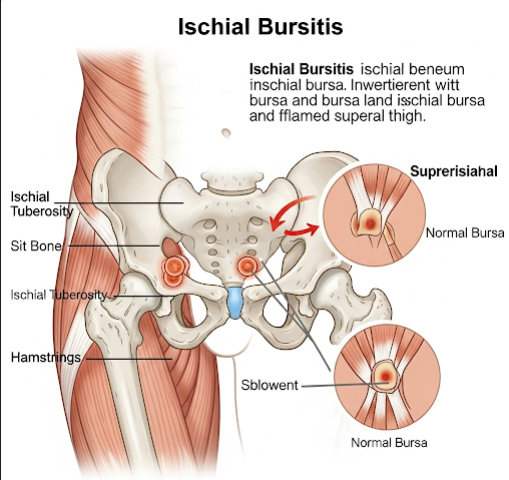
Ischial bursitis is an inflammatory disorder involving the ischial bursa, a small, fluid-filled sac located over the ischial tuberosity—the “sit bone” at the lower pelvis. This bursa functions to minimize friction between the ischial tuberosity and the overlying muscles, tendons (notably the hamstrings), and skin during movements such as sitting, walking, and running. When this bursa becomes irritated or inflamed, it leads to ischial bursitis, manifesting as localized pain and tenderness, especially when sitting or during hip movements. Though not very common, ischial bursitis can cause chronic discomfort and restrict mobility. In Korea, increasing awareness of musculoskeletal disorders and widespread access to advanced imaging and rehabilitative therapies contribute to effective diagnosis and treatment.
What is Ischial Bursitis?
Ischial bursitis involves inflammation of the bursa that lies between the ischial tuberosity and the adjacent soft tissues, including the hamstring origin and gluteal muscles. The ischial bursa acts as a cushion, absorbing stress from prolonged sitting and repetitive hip movements. However, excessive pressure, trauma, or repetitive micro-injuries can cause the bursa to become inflamed.
The inflamed bursa fills with excess fluid, thickens, and causes pain due to irritation of surrounding nerves and soft tissues. It is frequently associated with conditions such as hamstring tendinopathy or sciatica and can be mistaken for other causes of buttock pain, making clinical diagnosis challenging without imaging support.
Symptoms
The clinical presentation of ischial bursitis includes:
- Localized pain: Sharp or aching pain directly over the ischial tuberosity, which may radiate down the posterior thigh.
- Pain aggravated by sitting: Particularly on hard surfaces, causing discomfort and forcing patients to shift position frequently or avoid sitting.
- Tenderness: Palpation over the ischial tuberosity elicits localized tenderness and sometimes swelling or a palpable mass.
- Discomfort with hip movement: Activities involving hip extension such as climbing stairs, running, or standing up from a seated position worsen the pain.
- Stiffness and reduced hip flexibility: Chronic inflammation may limit range of motion.
- Night pain: Some patients experience pain that disturbs sleep, especially when lying on the affected side.
- Possible signs of inflammation: Warmth or redness over the area in acute cases, though rare.
Causes
Ischial bursitis results from multiple possible causes, often related to repetitive stress or direct injury:
- Prolonged sitting on hard surfaces: Mechanical pressure compresses the bursa against the ischial tuberosity, leading to irritation and inflammation. This is common in occupations or hobbies involving extended sitting such as driving, sewing, or cycling.
- Repetitive hip motion: Sports like running, rowing, and cycling cause repetitive hip extension and flexion that can overload the bursa and the hamstring origin.
- Direct trauma: Falls or blunt injury to the buttock can damage the bursa and surrounding tissues.
- Hamstring tendinopathy or tears: Close anatomical relationship between the hamstring tendons and the bursa means injury to one often affects the other.
- Poor biomechanics and posture: Muscle imbalances, leg length discrepancies, or improper sitting posture can increase pressure on the ischial tuberosity.
- Obesity: Excess body weight increases mechanical load on pelvic structures during sitting.
- Inflammatory or systemic diseases: Rarely, conditions such as rheumatoid arthritis, gout, or infection may trigger bursal inflammation.
Risk Factors
- Occupations involving prolonged sitting, especially on hard or firm seats (drivers, office workers, tailors).
- Athletes engaged in activities requiring repetitive hip extension and flexion.
- History of trauma to the pelvic region.
- Anatomical variations causing increased pressure on the ischial tuberosity.
- Excess body weight or obesity.
- Sedentary lifestyle combined with sudden increases in physical activity.
- Poor ergonomic setup at workplaces or during sports.
Complications
If ischial bursitis is left untreated or subjected to ongoing mechanical stress, complications may arise:
- Chronic pain: Persistent discomfort can affect mobility, work capacity, and quality of life.
- Bursal thickening and fibrosis: Repeated inflammation leads to scarring and decreased bursal elasticity.
- Cyst formation: Fluid accumulation within the bursa may form palpable cysts causing discomfort.
- Secondary hamstring injuries: Chronic inflammation can weaken or damage hamstring tendons.
- Infection: Although rare, septic bursitis can develop if bacteria invade the bursa through trauma or skin infections. This requires urgent treatment.
- Altered gait and posture: Compensation for pain can lead to secondary musculoskeletal problems.
Prevention
- Avoid prolonged sitting on hard or unpadded surfaces; use cushioned or ergonomically designed seating.
- Take frequent breaks during extended sitting periods to relieve pressure.
- Maintain good posture with hips properly aligned while sitting.
- Perform regular stretching and strengthening exercises for the hips, gluteal muscles, and hamstrings.
- Gradually increase intensity and duration of physical activities to prevent overload.
- Maintain healthy body weight to reduce mechanical stress.
- Use appropriate sports techniques and protective equipment.
- Early consultation for persistent buttock pain to initiate treatment promptly.
Treatment Options in Korea
Korean healthcare offers a range of effective, evidence-based treatments for ischial bursitis combining conventional and integrative approaches:
- Clinical diagnosis: Based on detailed history and physical examination focusing on pain localization and aggravating factors.
- Imaging: Ultrasound is commonly used to detect bursal inflammation and fluid accumulation; MRI provides detailed views of soft tissues and can identify associated hamstring or pelvic pathology.
- Conservative management:
- Rest and activity modification to reduce pressure and allow inflammation to subside.
- Application of ice packs initially to reduce swelling, followed by heat therapy to relax muscles.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to alleviate pain and inflammation.
- Physical therapy emphasizing stretching, strengthening, postural correction, and ergonomic advice.
- Use of padded cushions or donut pillows during sitting to offload pressure on the ischial tuberosity.
- Interventional treatments:
- Ultrasound-guided corticosteroid injections into the bursa for refractory or severe inflammation, offering rapid symptom relief.
- Aspiration of fluid collections if significant swelling or cyst formation occurs.
- Surgical intervention: Rarely required; reserved for cases with persistent symptoms unresponsive to conservative and interventional treatments, or when infection or other structural abnormalities necessitate bursa excision.
- Integrative therapies: Many patients in Korea also benefit from traditional treatments such as acupuncture and herbal medicine, which can complement conventional care to reduce inflammation and improve healing.