Overview
Ischemic stroke is a medical emergency caused by the sudden blockage of a blood vessel supplying the brain, leading to oxygen deprivation and death of brain tissue in the affected area. It represents approximately 80–85% of all stroke cases globally, including in Korea, where stroke remains a leading cause of adult disability and death. The brain is highly sensitive to interruptions in blood flow, and even brief ischemia can result in irreversible neurological damage. The rapid identification and management of ischemic stroke are crucial to reduce brain injury and improve patient outcomes. Korea has developed a sophisticated stroke care system involving early recognition, prompt reperfusion therapy, comprehensive acute care, and multidisciplinary rehabilitation, significantly improving survival and recovery rates.
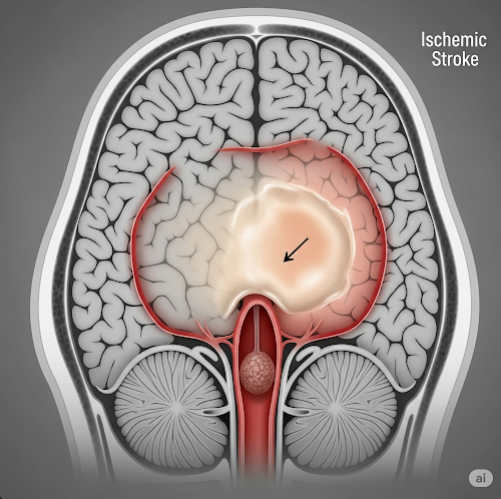
What is Ischemic Stroke?
Ischemic stroke occurs when an artery supplying the brain becomes occluded by a blood clot (thrombus) forming locally or an embolus traveling from elsewhere, most commonly the heart. This blockage disrupts cerebral blood flow, causing deprivation of oxygen and nutrients to the brain tissue downstream. The lack of oxygen leads to cell death (infarction) and subsequent neurological deficits depending on the brain region involved.
Ischemic strokes are classified based on etiology and size:
- Large artery atherosclerosis: Occlusion or narrowing of major cerebral arteries or carotid arteries due to atherosclerotic plaques.
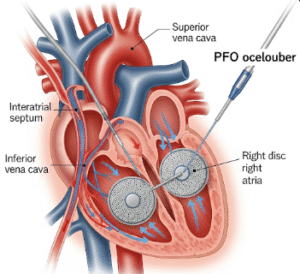
- Cardioembolism: Emboli arising from cardiac sources such as atrial fibrillation, myocardial infarction, prosthetic heart valves, or infective endocarditis.
- Small vessel disease (lacunar infarcts): Occlusion of small penetrating arteries typically due to chronic hypertension or diabetes.
- Other causes: Arterial dissection, vasculitis, hypercoagulable states, or unknown causes (cryptogenic stroke).
Symptoms
The clinical presentation of ischemic stroke is sudden and depends on the brain area affected:
- Motor deficits: Sudden weakness or paralysis (hemiparesis or hemiplegia), usually affecting one side of the body, including face, arm, and leg.
- Sensory disturbances: Numbness or loss of sensation on one side.
- Speech impairment: Difficulty speaking (expressive aphasia), understanding language (receptive aphasia), or slurred speech (dysarthria).
- Visual disturbances: Loss of vision in one or both eyes, visual field defects such as hemianopia.
- Coordination and balance problems: Dizziness, ataxia, or difficulty walking.
- Altered consciousness: Ranging from confusion to coma in severe strokes.
- Sudden severe headache: Less common in ischemic stroke but may occur.
The FAST mnemonic helps the public identify stroke symptoms: Face drooping, Arm weakness, Speech difficulty, Time to call emergency services.
Causes
Ischemic stroke develops due to obstruction of cerebral blood vessels:
- Atherosclerosis: Plaque buildup leads to vessel narrowing, thrombosis, and embolization.
- Cardiac embolism: Atrial fibrillation is a major source of emboli; clots formed in the heart’s left atrium or ventricle travel to cerebral arteries.
- Small vessel disease: Chronic hypertension and diabetes cause lipohyalinosis and microatheroma formation, occluding small penetrating arteries.
- Hypercoagulable states: Genetic or acquired disorders such as antiphospholipid syndrome or malignancy increase thrombosis risk.
- Arterial dissection: Tear in arterial wall leads to clot formation and embolism.
- Inflammatory vasculopathies: Vasculitis and other autoimmune conditions affecting cerebral vessels.
- Other risk factors: Smoking, obesity, sedentary lifestyle, and excessive alcohol use contribute indirectly by promoting atherosclerosis.
Risk Factors
- Non-modifiable:
- Increasing age (risk doubles every decade after 55).
- Male gender (though women have higher lifetime risk due to longevity).
- Family history of stroke or cardiovascular disease.
- Ethnicity (some populations have higher stroke prevalence).
- Modifiable:
- Hypertension (the single most important risk factor).
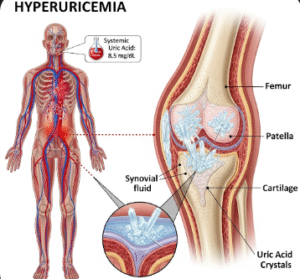
- Diabetes mellitus.
- Hyperlipidemia (high LDL cholesterol).
- Smoking.
- Obesity and physical inactivity.
- Atrial fibrillation and other cardiac diseases.
- Excessive alcohol consumption.
- Poor diet (high salt, saturated fat, and sugar intake).
- Stress and depression.
Complications
Ischemic stroke can lead to numerous serious complications:
- Neurological disabilities: Persistent weakness, paralysis, speech impairment, sensory deficits, and cognitive impairment.
- Emotional and psychological effects: Depression, anxiety, and social isolation.
- Seizures: Post-stroke epilepsy can develop.
- Swallowing difficulties: Risk of aspiration pneumonia.
- Deep vein thrombosis and pulmonary embolism: Due to immobility.
- Pressure sores: From prolonged bed rest.
- Recurrent strokes: Patients with one stroke are at high risk of subsequent strokes.
- Death: Particularly in large strokes or those with delayed treatment.
Prevention
Primary and secondary prevention strategies include:
- Blood pressure control: Keeping hypertension within target levels significantly reduces stroke risk.
- Glycemic control: Optimal diabetes management.
- Lipid lowering: Statins reduce atherosclerotic progression and stroke risk.
- Lifestyle modification: Smoking cessation, healthy diet rich in fruits, vegetables, and whole grains, regular physical activity, weight management, and limited alcohol.
- Management of atrial fibrillation: Use of anticoagulants such as warfarin or novel oral anticoagulants to prevent cardioembolism.
- Antiplatelet therapy: Aspirin or clopidogrel in high-risk patients for secondary prevention.
- Regular screening: Early identification and management of risk factors.
Treatment Options in Korea
Korea has established an advanced, integrated stroke care system encompassing prevention, acute management, and rehabilitation:
- Emergency response: Public education campaigns have improved early recognition and emergency calls for stroke symptoms.
- Imaging: Rapid brain CT and MRI scans to differentiate ischemic from hemorrhagic stroke and assess salvageable brain tissue.
- Intravenous thrombolysis: Administration of recombinant tissue plasminogen activator (tPA) within 4.5 hours of symptom onset dissolves clots and restores perfusion.
- Endovascular thrombectomy: Mechanical removal of large vessel clots via catheter techniques, extending treatment window up to 24 hours for eligible patients.
- Neurocritical care: Monitoring and managing cerebral edema, intracranial pressure, blood pressure, oxygenation, and preventing complications.
- Secondary prevention: Long-term use of antiplatelets, anticoagulants, statins, and control of comorbidities.
- Multidisciplinary rehabilitation: Physical therapy, occupational therapy, speech therapy, and psychological support improve functional recovery and quality of life.
- Stroke centers and networks: Designated hospitals provide specialized care with standardized protocols and seamless transfer systems.