Overview
Isolated systolic hypertension (ISH) is a common form of high blood pressure characterized by an elevated systolic blood pressure (the top number) above 130 mmHg while the diastolic pressure (the bottom number) remains below 80 mmHg. It primarily affects older adults but can occur at any age. ISH is a significant cardiovascular risk factor linked to an increased likelihood of heart attack, stroke, kidney disease, and other complications. In Korea, where the aging population is growing, awareness, diagnosis, and management of ISH are crucial to reduce cardiovascular morbidity and mortality. Advances in healthcare have made effective treatment and monitoring accessible throughout the country.
What is Isolated Systolic Hypertension?
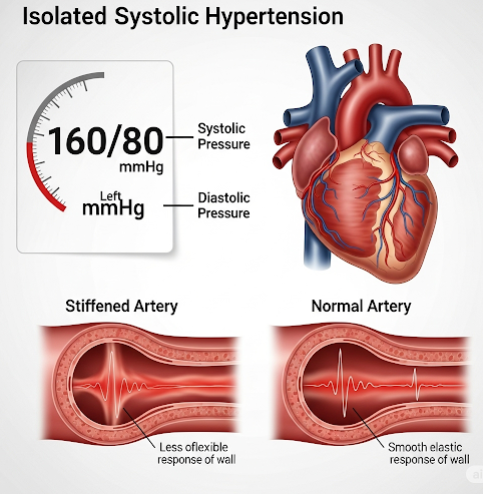
Isolated systolic hypertension occurs when only the systolic blood pressure—the pressure in arteries during heartbeats—is elevated, while diastolic blood pressure—the pressure between heartbeats—remains normal or low. Normally, both values rise or fall together, but in ISH, the stiffening of large arteries, especially the aorta, leads to increased systolic pressure.
This condition is distinct from combined hypertension (where both systolic and diastolic are elevated) and poses unique risks. ISH reflects increased arterial stiffness and reduced vascular compliance, making the heart work harder and increasing strain on vital organs.
Symptoms
ISH itself often does not produce noticeable symptoms, earning it the label “silent killer.” However, some patients may experience symptoms related to elevated blood pressure or its complications:
- Headaches or dizziness.
- Fatigue or confusion.
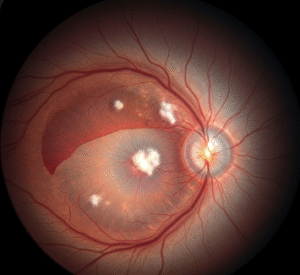
- Visual disturbances.
- Chest pain or palpitations (if heart involvement occurs).
- Nosebleeds (rare and usually when blood pressure is severely elevated).
- Shortness of breath during exertion.
Often, symptoms appear only after significant organ damage has occurred, underscoring the importance of regular blood pressure screening.
Causes
ISH results mainly from changes in the arterial system associated with aging and other health factors:
- Arterial stiffness: With aging, large arteries lose elasticity due to structural changes in the vessel walls, such as collagen buildup and calcium deposits (arteriosclerosis).
- Atherosclerosis: Plaque buildup narrows arteries, further reducing their compliance.
- Increased cardiac output: Conditions like hyperthyroidism or anemia can increase systolic pressure.
- Lifestyle factors: Obesity, high salt intake, and sedentary lifestyle contribute indirectly by accelerating vascular damage.
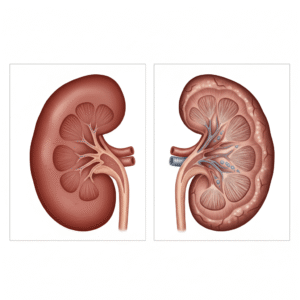
- Chronic kidney disease: Impairs fluid and pressure regulation.
- Other causes: Sleep apnea, excessive alcohol consumption, and certain medications.
Risk Factors
- Age (most common in people over 60).
- Male sex, although post-menopausal women catch up in risk.
- Family history of hypertension or cardiovascular disease.
- Obesity and metabolic syndrome.
- Sedentary lifestyle and poor diet (high sodium, low potassium).
- Smoking.
- Diabetes mellitus.
- Chronic kidney disease.
- Stress and excessive alcohol use.
Complications
If untreated, ISH can lead to serious health consequences:
- Heart disease: Left ventricular hypertrophy (thickening of the heart muscle), heart failure, coronary artery disease.
- Stroke: Increased risk of ischemic and hemorrhagic strokes.
- Kidney damage: Hypertensive nephropathy leading to chronic kidney disease.
- Aneurysms: Formation of artery wall bulges that may rupture.
- Cognitive decline: Higher risk of vascular dementia and Alzheimer’s disease.
- Vision loss: Hypertensive retinopathy damaging retinal vessels.
Prevention
- Regular blood pressure screening, especially for those over 50.
- Maintaining healthy body weight and waist circumference.
- Balanced diet rich in fruits, vegetables, whole grains, and low in sodium.
- Regular physical activity (150 minutes per week of moderate exercise recommended).
- Smoking cessation and moderation of alcohol consumption.
- Stress management techniques such as meditation or yoga.
- Adequate sleep and management of sleep apnea if present.
- Control of diabetes and lipid abnormalities.
Treatment Options in Korea
Management of ISH in Korea focuses on lifestyle modification combined with medication when necessary:
- Lifestyle changes:
- Diet: Adoption of DASH (Dietary Approaches to Stop Hypertension) diet, reducing salt intake to less than 2,300 mg/day.
- Exercise: Regular aerobic activities such as walking, cycling, or swimming.
- Weight loss in overweight individuals.
- Smoking cessation programs and alcohol moderation.
- Pharmacologic treatment:
- Calcium channel blockers (e.g., amlodipine) and thiazide diuretics are often first-line treatments, as they effectively lower systolic pressure.
- ACE inhibitors or ARBs may be used, especially if there are comorbidities such as diabetes or kidney disease.
- Beta-blockers are less favored unless there is a specific cardiac indication.
- Combination therapy may be required for adequate control.
- Regular monitoring:
- Frequent blood pressure checks to assess treatment efficacy and adjust medications.
- Monitoring for potential side effects.
- Screening for complications such as kidney function tests and eye exams.
- Public health initiatives:
- Korea’s national health programs promote awareness of hypertension and cardiovascular risk.
- Access to community-based screening and counseling.
- Integration of traditional Korean medicine options for complementary care.