Overview
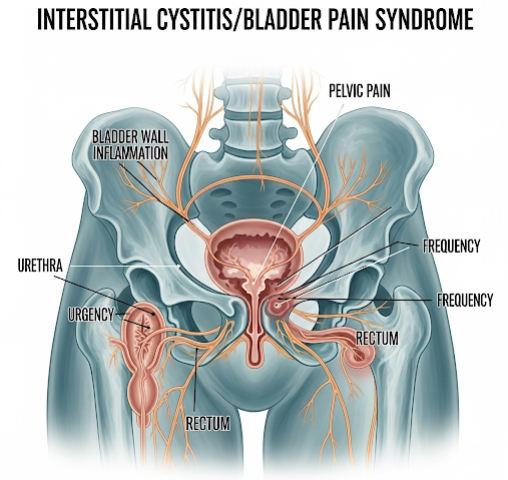
Interstitial Cystitis (IC), also called Bladder Pain Syndrome (BPS), is a chronic condition characterized by bladder pain, urinary urgency, frequency, and discomfort. Unlike typical urinary tract infections, IC/BPS is not caused by bacteria but involves inflammation or irritation of the bladder wall, leading to persistent pelvic pain and urinary symptoms. This condition significantly affects the quality of life, causing physical discomfort, sleep disturbances, and emotional distress.
In Korea, awareness of IC/BPS has increased with advances in urological diagnostics and treatments, including innovative therapies and integrative medicine approaches. Korean medical centers specialize in multidisciplinary management to improve patient outcomes.
What is Interstitial Cystitis/Bladder Pain Syndrome?
IC/BPS is a complex syndrome involving chronic inflammation of the bladder’s mucosal lining, causing pain and lower urinary tract symptoms without evidence of infection or other identifiable causes. The exact cause remains unclear but may involve bladder epithelial dysfunction, immune responses, nerve hypersensitivity, or autoimmune components. Patients often experience a combination of pelvic pain, urinary urgency, and frequency, which can vary in severity over time.
Symptoms
Common symptoms of IC/BPS include:
- Persistent pain or pressure in the bladder, pelvic area, or lower abdomen
- Frequent urination, often more than 8 times during the day and sometimes at night (nocturia)
- Urgency to urinate, often with little urine output
- Pain during sexual intercourse (dyspareunia)
- Discomfort or burning sensation during urination
- Episodes of symptom flare-ups triggered by stress, diet, or hormonal changes
- Some patients may also report fatigue, sleep disturbances, or mood disorders due to chronic pain
Causes
The precise cause of IC/BPS is not fully understood, but several theories exist:
- Bladder epithelial dysfunction: Damage to the bladder lining allows irritants in the urine to penetrate deeper tissues.
- Autoimmune factors: The body’s immune system may mistakenly attack bladder tissue.
- Neurogenic inflammation: Increased sensitivity and abnormal nerve signaling cause pain.
- Genetic predisposition: Family history may play a role.
- Infections or trauma: Previous urinary infections or bladder injury may contribute.
Risk Factors
Certain factors increase the risk of developing IC/BPS:
- Female gender: Women are affected far more often than men.
- Age: Most patients are diagnosed in middle age but symptoms can appear earlier.
- History of urinary tract infections or bladder trauma.
- Autoimmune diseases such as lupus or rheumatoid arthritis.
- Allergies or other chronic pain syndromes like fibromyalgia.
- Stress and psychological factors may exacerbate symptoms.
Complications
If untreated or poorly managed, IC/BPS can lead to:
- Chronic pelvic pain and reduced quality of life
- Sexual dysfunction and relationship difficulties
- Urinary retention or incomplete bladder emptying
- Psychological issues including anxiety and depression
- Social isolation due to frequent bathroom needs and pain
Prevention
Prevention is challenging because the exact cause is unclear, but patients can reduce symptoms and flare-ups by:
- Avoiding known dietary irritants such as caffeine, alcohol, spicy foods, and artificial sweeteners
- Managing stress through relaxation techniques, counseling, or physical therapies
- Maintaining proper hydration but avoiding excessive fluid intake
- Practicing good bladder habits to avoid irritation
- Early treatment of urinary infections or bladder injuries
Treatment Options in Korea
Diagnosis
Diagnosis of IC/BPS in Korea involves:
- Detailed patient history and symptom assessment
- Urinalysis and urine cultures to exclude infection
- Cystoscopy with hydrodistention to examine bladder lining and identify characteristic changes
- Urodynamic studies to assess bladder function
- Pain and symptom questionnaires for comprehensive evaluation
Medical Management
- Oral medications including pentosan polysulfate sodium (Elmiron), antihistamines, tricyclic antidepressants, and pain relievers
- Intravesical therapies where medications are directly instilled into the bladder to reduce inflammation
- Antibiotics are generally avoided unless there is a concurrent infection
- Korean urologists often combine Western medical treatments with traditional herbal medicines tailored to patient needs
Physical and Behavioral Therapies
- Pelvic floor physical therapy to relieve muscle spasms and improve bladder function
- Bladder training and timed voiding techniques
- Stress management and cognitive behavioral therapy (CBT) to address the psychological aspects of chronic pain
Surgical Treatment
Surgery is rare and reserved for severe, refractory cases and may include procedures like bladder augmentation or nerve ablation. Korean surgeons have experience in minimally invasive approaches when surgery is necessary.
Integrative and Complementary Therapies
- Acupuncture and moxibustion are commonly used in Korea alongside conventional treatments to relieve pain and improve symptoms.
- Dietary counseling and lifestyle modification programs tailored to Korean dietary habits are part of comprehensive care.
Prognosis in Korea
While there is no definitive cure for IC/BPS, most patients in Korea experience symptom improvement with a combination of treatments tailored to their condition. Early diagnosis and multidisciplinary care at specialized urology centers contribute to better quality of life and reduced symptom burden. Continuous research and increasing patient awareness also support improved management strategies in Korea.