Overview
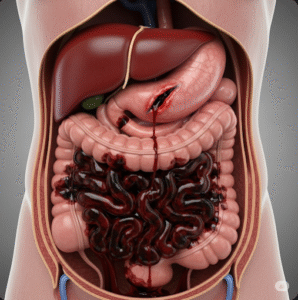
Intestinal Ischemic Syndrome, also known as intestinal ischemia or mesenteric ischemia, is a serious medical condition where blood flow to the intestines is reduced or blocked. This reduction in blood supply can cause tissue damage, inflammation, and if untreated, can lead to life-threatening complications such as bowel necrosis. Prompt diagnosis and treatment are crucial to improve outcomes. In Korea, advances in diagnostic imaging and interventional procedures have significantly enhanced the management of intestinal ischemic syndrome, making it a critical focus in emergency and gastroenterological care.
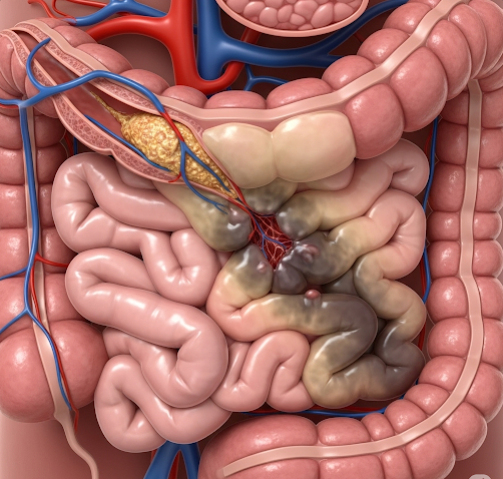
What is Intestinal Ischemic Syndrome?
Intestinal Ischemic Syndrome refers to insufficient blood flow to the small or large intestines, leading to a lack of oxygen and nutrients required for normal function. The condition can affect any part of the intestine but is most commonly seen in the small intestine and the colon.
The syndrome can be acute or chronic:
- Acute intestinal ischemia occurs suddenly, often due to a blood clot or embolism blocking the arteries supplying the intestines.
- Chronic intestinal ischemia develops gradually from narrowed arteries due to atherosclerosis (plaque buildup).
Without adequate blood flow, the intestinal tissues suffer damage that can progress to inflammation, ulcers, and tissue death (necrosis), which can result in perforation and peritonitis—a life-threatening infection of the abdominal cavity.
Symptoms
Symptoms of intestinal ischemic syndrome vary depending on whether the condition is acute or chronic, but generally include:
- Severe abdominal pain: Often sudden and out of proportion to physical findings in acute cases. Pain may be diffuse or localized.
- Nausea and vomiting: Common, especially in acute ischemia.
- Diarrhea or bloody stools: Indicate mucosal injury and inflammation.
- Abdominal tenderness: May develop as the condition progresses.
- Weight loss and fear of eating: Seen in chronic ischemia due to post-meal pain.
- Fever and signs of infection: Possible if bowel necrosis or perforation occurs.
- Shock: In severe cases, due to systemic infection or blood loss.
Causes
The causes of intestinal ischemic syndrome can be broadly categorized into arterial, venous, and non-occlusive types:
- Arterial occlusion: Blockage of the mesenteric arteries by embolism (e.g., from the heart in atrial fibrillation) or thrombosis (clot formation in narrowed arteries).
- Venous thrombosis: Clot in the mesenteric veins leading to impaired blood drainage and ischemia.
- Non-occlusive ischemia: Reduced blood flow due to low cardiac output, shock, or vasoconstriction without a physical blockage.
- Atherosclerosis: Chronic narrowing of arteries causing reduced blood supply over time.
- Other causes: Vasculitis, trauma, or surgical complications.
Risk Factors
Several factors increase the risk of developing intestinal ischemic syndrome:
- Age: More common in older adults.
- Cardiovascular disease: Including atrial fibrillation, heart failure, and atherosclerosis.
- Hypercoagulable states: Conditions that increase blood clotting tendency.
- Smoking: Accelerates arterial disease.
- Diabetes and hypertension: Contribute to vascular damage.
- Recent abdominal surgery or trauma: Can predispose to thrombosis.
- Use of vasoconstrictive medications: Such as digitalis or vasopressors.
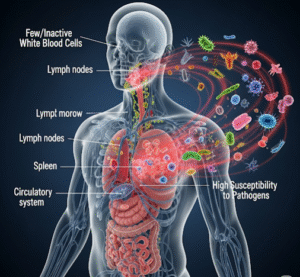
Complications
If untreated or delayed in diagnosis, intestinal ischemic syndrome can lead to serious complications:
- Bowel necrosis: Death of intestinal tissue requiring emergency surgery.
- Perforation: Hole in the intestine causing leakage of contents into the abdominal cavity.
- Peritonitis: Severe infection and inflammation of the abdominal lining.
- Sepsis: Life-threatening systemic infection.
- Chronic intestinal dysfunction: Resulting in malabsorption or strictures.
- Death: Due to complications or multi-organ failure.
Prevention
Preventing intestinal ischemic syndrome involves managing underlying risk factors:
- Control cardiovascular diseases: Effective management of atrial fibrillation, hypertension, and atherosclerosis.
- Avoid smoking: To reduce vascular disease progression.
- Maintain healthy lifestyle: Balanced diet, regular exercise, and weight control.
- Manage diabetes: Strict blood sugar control reduces vascular complications.
- Medications: Use blood thinners or antiplatelet drugs as prescribed to prevent clots.
- Regular check-ups: For high-risk individuals to monitor vascular health.
Treatment Options in Korea
Korea provides advanced medical care for intestinal ischemic syndrome with rapid diagnosis and multidisciplinary treatment approaches:
- Diagnosis:
High-resolution CT angiography is widely available in Korean hospitals and is the gold standard for diagnosing intestinal ischemia. Additional tests may include blood work to assess for infection and ischemic damage, and sometimes endoscopy. - Medical Management:
- Stabilization with intravenous fluids, oxygen, and pain control.
- Antibiotics to prevent or treat infection.
- Anticoagulants to dissolve or prevent clots in venous thrombosis.
- Vasodilators in non-occlusive ischemia to improve blood flow.
- Interventional Radiology:
Korean hospitals offer minimally invasive procedures such as angioplasty or stenting to open narrowed arteries and restore blood flow. - Surgical Treatment:
Surgery may be required to remove necrotic bowel segments or bypass blocked arteries. Korean surgical teams are highly skilled in both open and laparoscopic techniques for this purpose. - Postoperative Care and Rehabilitation:
Intensive monitoring, nutritional support, and rehabilitation are integral parts of recovery. - Follow-up:
Regular follow-up with gastroenterologists and vascular specialists to monitor for recurrence and manage cardiovascular risk.