Overview
Acute Kidney Injury (AKI), formerly known as acute renal failure, is a sudden loss of kidney function that occurs over hours or days. It causes a dangerous buildup of waste products, fluid, and electrolytes in the body. AKI is a medical emergency and often occurs in hospitalized patients, especially those in intensive care. Early diagnosis and treatment are crucial for recovery and preventing permanent kidney damage.
What is Acute Kidney Injury?
Acute Kidney Injury is a condition where the kidneys lose their filtering ability suddenly. This leads to accumulation of toxins, imbalances in fluid and electrolytes, and disruptions in other organ functions. AKI can be reversible if treated promptly, but in severe cases, it may result in chronic kidney disease or require dialysis.
There are three major types of AKI, depending on the underlying cause:
- Pre-renal AKI – due to reduced blood flow to the kidneys
- Intrinsic AKI – due to direct kidney damage (e.g., inflammation or toxins)
- Post-renal AKI – due to obstruction of urine outflow
Symptoms
Symptoms of AKI can vary depending on severity but may include:
- Decreased urine output (oliguria)
- Swelling in legs, ankles, or around the eyes
- Fatigue or drowsiness
- Shortness of breath
- Nausea and vomiting
- Confusion or altered mental status
- Chest pain or pressure (in severe fluid overload)
- Seizures or coma (in severe cases)
Sometimes, there may be no symptoms, especially in early stages.
Causes
AKI can result from a wide variety of conditions. Common causes include:
Pre-renal Causes (most common):
- Severe dehydration
- Blood loss or shock
- Heart failure
- Liver failure
- Sepsis
Intrinsic Causes:
- Acute tubular necrosis (from toxins or ischemia)
- Glomerulonephritis
- Interstitial nephritis (from drugs or infections)
- Autoimmune diseases (e.g., lupus)
Post-renal Causes:
- Kidney stones
- Enlarged prostate (BPH)
- Bladder tumors
- Ureteral obstruction
Risk Factors
Certain individuals are at higher risk of developing AKI, including those with:
- Pre-existing chronic kidney disease (CKD)
- Diabetes or hypertension
- Heart failure or liver disease
- Older age (60+)
- Recent surgery or hospitalization
- Use of nephrotoxic drugs (NSAIDs, contrast dyes, some antibiotics)
- Severe infections or sepsis
Complications
If not managed properly, AKI can lead to serious complications, such as:
- Fluid overload (leading to pulmonary edema)
- High potassium levels (hyperkalemia) – life-threatening
- Metabolic acidosis
- Uremia (toxic buildup of waste)
- Anemia
- Permanent kidney damage or chronic kidney disease
- Need for long-term dialysis
- Death (especially in critically ill patients)
Prevention
Preventing AKI involves identifying and minimizing risk factors, particularly in hospitalized or vulnerable individuals:
- Stay well hydrated, especially during illness or heat
- Avoid overuse of NSAIDs or contrast dyes
- Monitor kidney function in high-risk patients (e.g., diabetics)
- Manage underlying conditions like diabetes, hypertension, and heart failure
- Promptly treat infections or sepsis
- Monitor medications in elderly or those with CKD
Treatment Options Korea
1. Hospital Admission and Monitoring
- Most moderate to severe AKI cases are managed in inpatient settings
- Admitted to nephrology, internal medicine, or intensive care units (ICU) if unstable
- Monitoring includes:
- Serum creatinine and BUN
- Electrolytes (K⁺, Na⁺, Ca²⁺)
- Urine output and urinalysis
2. Identify and Treat the Underlying Cause
- Prerenal AKI: treat dehydration, blood loss, or hypotension
- Intrinsic AKI: stop nephrotoxic agents (e.g., NSAIDs, contrast), treat glomerular or tubular injury
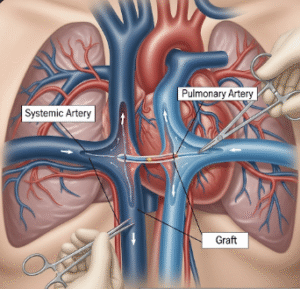
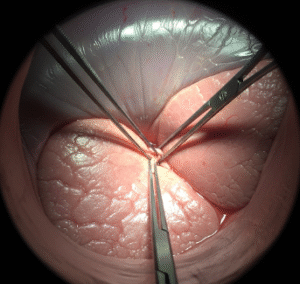
- Postrenal AKI: relieve obstruction via catheterization or surgical intervention
3. Fluid and Electrolyte Management
- Careful IV fluid replacement or diuresis depending on volume status
- Avoid fluid overload—may use loop diuretics (e.g., furosemide) if necessary
- Manage hyperkalemia, acidosis, and hyponatremia
4. Renal Replacement Therapy (Dialysis)
- Indicated if:
- Severe electrolyte imbalance (esp. hyperkalemia)
- Volume overload
- Uremic symptoms (e.g., pericarditis, confusion)
- Severe acidosis
- Options include intermittent hemodialysis, continuous renal replacement therapy (CRRT) in ICUs
- Available at nephrology departments in all major Korean hospitals
5. Medication Adjustment
- Dosing of all medications is adjusted based on estimated glomerular filtration rate (eGFR)
- Avoidance of nephrotoxic drugs (e.g., aminoglycosides, contrast agents)
6. Nutritional and Supportive Care
- Renal diet: low sodium, potassium, and phosphate
- Nutrition support provided by trained dietitians in Korean hospitals
- Anemia management if needed
7. Long-Term Follow-Up
- Monitor for recovery vs. progression to chronic kidney disease (CKD)
- Regular nephrology follow-ups
- Education on kidney health, lifestyle, and early symptom recognition
Final Thoughts
Acute Kidney Injury is a serious and potentially life-threatening condition, especially in hospitalized or critically ill individuals. With prompt recognition, appropriate treatment, and careful monitoring, many patients recover full or partial kidney function. Public awareness and healthcare vigilance are essential in preventing long-term complications or death.