Overview
Ocular albinism (OA) is a rare, genetic condition that primarily affects the eyes, resulting in reduced pigmentation of the iris and retina. This leads to visual problems, such as decreased sharpness of vision, light sensitivity, and involuntary eye movements. Unlike oculocutaneous albinism (which affects the skin, hair, and eyes), ocular albinism mostly impacts the eyes alone, with little or no change in skin or hair pigmentation.
It is most commonly passed down through an X-linked recessive inheritance pattern, meaning it predominantly affects males, while females are typically carriers.
What is Ocular Albinism?
Ocular albinism is caused by mutations in genes that regulate the production and distribution of melanin, the pigment that gives color to the eyes. Melanin is essential for the normal development of the retina and optic nerves, which means people with OA have impaired vision due to structural abnormalities.
The most common type is Ocular Albinism Type 1 (OA1), caused by a mutation in the GPR143 gene. This condition is present at birth and is non-progressive, though visual symptoms typically last a lifetime.
Symptoms
Symptoms of ocular albinism can vary depending on the severity, but often include:
- Reduced visual acuity (blurred or poor vision)
- Nystagmus (involuntary side-to-side eye movements)
- Photophobia (sensitivity to light)
- Strabismus (crossed or misaligned eyes)
- Poor depth perception
- Foveal hypoplasia (underdevelopment of the central retina)
- Translucent iris (appears light-colored and may glow under bright light)
Most individuals have normal skin and hair color, though they may be slightly lighter than family members.
Causes
Ocular albinism is primarily caused by mutations in the GPR143 gene, which is located on the X chromosome. This gene plays a critical role in the development and function of pigment cells in the eyes.
The mutation leads to melanin deficiency in the retina and other parts of the eye, which disrupts visual pathway development between the eye and brain.
Other rarer forms of ocular albinism may be associated with autosomal recessive inheritance or part of syndromes involving multiple body systems.
Risk Factors
Risk factors for ocular albinism include:
- Family history of ocular albinism or related genetic disorders
- Being male (due to X-linked inheritance)
- Having parents who are carriers of the gene mutation
- Belonging to a family with a known X-linked genetic condition
In most cases, a person is born with OA, and it is diagnosed in infancy or early childhood.
Complications
Ocular albinism can lead to a number of complications if not managed properly:
- Persistent visual impairment
- Educational challenges due to visual limitations
- Difficulty with activities requiring fine vision
- Social or emotional effects, especially in school-aged children
- Risk of being misdiagnosed or misunderstood without visible albinism traits
With proper visual aids and accommodations, most individuals can lead independent and fulfilling lives.
Prevention
Ocular albinism cannot be prevented, as it is a genetic disorder, but several steps can support early diagnosis and management:
- Genetic counseling for families with a history of the condition
- Prenatal testing (in families with known mutations)
- Early eye exams for infants with unusual eye movements or poor vision
- Avoiding excessive sun exposure, especially for children with light sensitivity
Early detection and supportive care can significantly improve quality of life.
Treatment Options in Korea
While there is no cure for ocular albinism, South Korea offers advanced eye care and vision rehabilitation services that help manage symptoms and support visual development.
1. Diagnosis
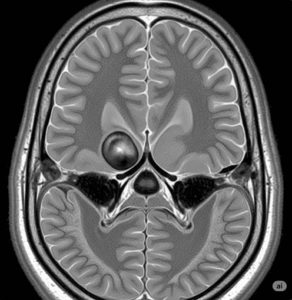
- Ophthalmologic examination: To assess visual acuity, eye movement, and eye alignment
- Electroretinography (ERG): Measures retinal response to light
- Visual evoked potential (VEP): Tests how signals travel from the retina to the brain
- Optical coherence tomography (OCT): Evaluates retinal structure
- Genetic testing: Confirms the diagnosis and determines inheritance patterns
2. Vision Support and Management
- Prescription glasses or contact lenses to improve visual acuity
- Low vision aids: Magnifiers, text-to-speech devices, and adaptive technologies
- Sunglasses or photochromic lenses to manage photophobia
- Nystagmus management: Includes eye muscle surgery in some cases
- Vision therapy and special education services for children
3. Genetic Counseling
- Support for families regarding inheritance, future pregnancies, and testing of relatives
- Carrier testing for female family members
4. Supportive Care
- Occupational therapy for visual-motor coordination
- School accommodations (large print books, seating arrangements)
- Psychological counseling, if needed, for coping with vision challenges
5. Top Hospitals and Vision Centers in Korea
- Severance Eye Hospital (Yonsei University Health System)
- Samsung Medical Center – Department of Pediatric Ophthalmology
- Asan Medical Center – Department of Ophthalmology and Genetics
- Seoul National University Hospital – Visual Rehabilitation Center
- CHA Bundang Medical Center – Pediatric Eye Clinic
These institutions offer:
- Advanced diagnostic and imaging technology
- Integrated genetic and ophthalmologic care
- Child-friendly vision rehabilitation programs
- Multilingual services for international families